Opinion
Why we need to prioritise sustainability in female health products
By Jo Barnard, founder and creative director at Morrama

Abingdon Health is proud to work in partnership with a number of female-led entrepreneurs. Here, Jo Barnard, founder of the certified B-Corp industrial design agency Morrama, discusses with us why companies should prioritise sustainability in the design of female health products.
When it comes to healthcare, considering sustainability can often drop down the list of priorities. With strict regulations and testing requirements, simply developing a product that works and gets approved for launch may be enough for most companies in the industry.
However, we are no longer in a situation where the planet can wait. Exacerbated by the pandemic, medical waste is threatening human and environmental health. So what can be done?
Designing for appropriate lifespan
We need to start at the end.
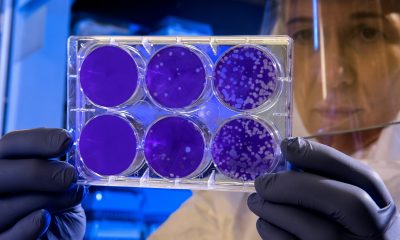
In the case of single or short-term use products such as rapid diagnostics tests, what happens at disposal is key. Where products that could be passed on or reused are concerned, then it’s important to consider safe re-use or refurbishment as an option.
By mapping out the full product lifecycle from beginning to end, we can design for more sustainable options without compromising on the user experience.
The real cost of materials
If you are designing a product to be used once, such as a pregnancy test, then cheap(est) materials may seem like the way to go, but using materials that will last hundreds of years no longer makes sense.
Our reliance on plastic, particularly within the healthcare market, is going to take some work to overcome, but we have to try.
The first step we can take is switching to biodegradable materials where we can. Particularly in healthcare and diagnostics where recycling isn’t an option, ensuring that the product will break down naturally is key to reducing waste. Materials such as PHA, starch-based biopolymers and new paper technologies all provide some exciting options.
FLUUS’s flushable sanitary pads are a great example. Period products are a huge contributor to single use plastic waste, so it’s amazing to see some real innovation in this space.

London-based Fluus uses plant fibres and natural adhesives to make biodegradable, flushable pads
Rethinking ownership
With longer-term use products, the question is, how long are they actually used for?
When it comes to getting pregnant for example, a tech-based product solution such as the Mira hormone and ovulation tracker may only be used for three months.
However, a woman is going to wait at least three more months before she considers getting rid of the device or may keep hold of it a few years for next time. In that time however, many other women could have benefited from the product.
It’s commonplace in the health service for patients to be given a device to use for a period of time and then be expected to return it. (Although, a large percentage of devices will be ‘written off’ once issued based on the likelihood of actual return, so there is still work to do there.)
When it comes to consumer products, however, we tend to prefer ownership over lease models.
That being said, with cost of living increasing, the pressure is on for brands to be creative over getting customers on-board and this is a great opportunity to explore subscription-model usage of certain products – where the user ‘owns’ the product for the time it is needed and then it is returned to the pool for the next user to draw from – and also incentives for re-using/recycling/re-selling equipment to prolong their useful lifecycle.
User behaviour
In all cases, we need to consider human behaviour. Once you have put a product into the hands of the user, you no longer have 100 per cent control as to what happens to it. We have to think about what people are likely to do and how we can nudge them to do the right thing.
With regards to brands creating disposable eco-options for diagnostics, such as pregnancy test brand Hoopsy, there needs to be consideration for how to instil the same faith in a paper strip as a hopeful mother has in the all-singing, all-dancing electronic alternative.
Where recycling is an option, how can you be sure that the product will actually end up in the recycling bin?
Design and material choice alone isn’t enough. When it comes to creating sustainable solutions that work, there is as much work to do in brand, positioning and education.
All sides need to work together if we are to accelerate the move to more sustainable healthcare solutions. Individuals have a big part to play, not just as end-users, but as key players in organisations bringing new products to market in a design, development, manufacturing, sales or marketing capacity.
We have to acknowledge the environmental costs of doing the same things we always have and push for change. That change could look like a roadmap for incremental improvements or chasing innovative solutions to the bigger challenges; either way, we have to accelerate our efforts to ensuring the planet becomes a stakeholder in our product development.
Morrama is proud to partner with Abingdon Health to support its CDMO customers in the design of innovative lateral flow products and sustainable packaging.
We are also extremely supportive of the work Abingdon does to support women in STEM, with a workforce that’s over 54 per cent women and over 56 per cent of its leadership positions held by females.
Jo Barnard is founder and creative director of industrial design and innovation consultancy Morrama.

Wellness
The science behind the scar: What’s really in our period products

By Ruby Raut, founder and CEO, WUKA
Over the past year, headlines about “toxic period products” have been hard to ignore. Stories about PFAS, heavy metals, and hormone disruptors in pads, tampons, and underwear have sparked global concern, and for good reason. But behind the fear, there’s a scientific story worth understanding.
At the recent House of Lords event, “Have We Reached the Tipping Point for Toxic Period Products?”, researchers and policymakers came together to separate fact from panic. The truth is more nuanced: yes, chemicals and metals are present in some menstrual products, but understanding how much, where they come from, and what that means for our health is key to driving change that’s informed, not sensational.
What Scientists Have Found So Far
Dr Kathrin Schilling, an environmental health scientist at Columbia University, shared new research that tested 16 metals in menstrual products, including arsenic, cadmium, lead, and antimony, all known toxic substances linked to long-term health effects such as cardiovascular disease, kidney problems, and hormonal disruption.
The findings were striking:
- Non-organic products showed higher levels of lead and cadmium than organic ones.
- Some reusable and single-use products exceeded 30,000 nanograms per gram (ng/g) of antimony, a toxic metal commonly used in plastics manufacturing.
- Lead levels varied dramatically, some products contained 100× more than others.
To put this in perspective, even very small doses of lead can cause harm. The World Health Organization confirms there is no safe level of lead exposure. Chronic, low-level contact can gradually affect the nervous system and fertility. The same applies to arsenic, where countries have tightened drinking water limits from 10 µg/L to as low as 1 µg/L after learning that long-term exposure causes disease.
So while the numbers in menstrual products might sound tiny, what matters most is frequency and route of exposure. Menstrual products are used regularly and in contact with one of the body’s most absorbent tissues — the vaginal wall — where absorption is estimated to be 10–80× higher than through skin. Over decades of use, even low concentrations can add up.
Understanding PFAS — The “Forever Chemicals”
Alongside metals, PFAS (per- and polyfluoroalkyl substances) have become another major concern. These synthetic compounds are used for absorbency and stain resistance — but they don’t break down easily, earning the name “forever chemicals.”
They accumulate in soil, water, and the human body, and have been linked to reproductive issues, thyroid disease, and immune dysfunction. California recently became the first state to ban PFAS in menstrual products, while New York is pushing for broader restrictions that include heavy metals and hormone disruptors.
These international shifts signal a clear message: the world is moving towards stricter, transparency-first regulation — something the UK could soon follow.
Why It Matters for Our Bodies
It’s important to remember that our world is already filled with background exposure, from air pollution, processed food, and household plastics. We all live in a chemically complex environment. The key isn’t to fear every product but to understand which exposures matter most and how to minimise them.
Menstrual products are unique because of their intimate and repeated contact with the body. Even trace chemicals can bypass the body’s natural detox systems when absorbed vaginally. This doesn’t mean every product is dangerous, but it underscores why regular, independent testing and clear ingredient disclosure are essential.
Internal vs. External Exposure: Why It Makes a Difference
One of the least understood parts of this debate is the difference between internal and external products. A pad or period underwear sits on the skin; it can only transfer chemicals through surface contact. But products like tampons or menstrual cups are inserted directly into the vagina, an environment that absorbs substances 10–80 times more efficiently than normal skin.
That’s because the vaginal wall is highly vascular, full of small blood vessels, and it bypasses the liver, the organ that usually filters and detoxifies harmful substances. So when a chemical is absorbed vaginally, it goes straight into the bloodstream.
Yet, most testing and regulation still treat all menstrual products as if exposure happens through skin contact. There’s very little research separating the risk profiles of internal (tampons, cups, discs) versus external (pads, underwear) products. That’s why scientists like Dr Schilling emphasised the need for new safety standards that actually reflect how the body interacts with these materials, not just how a fabric performs in a laboratory test.
How Responsible Brands Are Responding
Some brands are already ahead of regulation.
At WUKA, we take this responsibility seriously. We are one of the very few period underwear brands with no PFAS detected in our products. Every batch is tested rigorously, both at source (in China) and again in the UK by Eurofins laboratories, an independent global testing agency.
We also screen for toxic chemicals, metals, and harmful finishes, ensuring that what touches your body is as safe as it is sustainable. As a founder, I always remind our team: I use our products myself. If I wouldn’t wear it, I wouldn’t make it for anyone else.
Our philosophy is simple, transparency builds trust. Consumers shouldn’t need a chemistry degree to choose a safe period product.
The Path Ahead
The science is clear: menstrual product safety deserves the same rigour as drinking water, cosmetics, or food. But we can also take heart, awareness is growing, data is expanding, and governments are beginning to act.
As policymakers push for international standards (through bodies like the ISO TC338 on menstrual products), and as responsible brands lead by example, the future of menstrual care looks safer, smarter, and far more transparent than the past.
This isn’t just about fear of toxins, it’s about empowering everyone who menstruates with knowledge and choice. Because understanding the science is the first step toward changing it.
Find out more about WUKA at wuka.co.uk
Features
How Westminster is finally talking about toxic period products

By Ruby Raut, founder and CEO, WUKA
For years, campaigners, scientists, and brands like ours have been calling attention to a hidden issue: the chemicals, metals, and toxins found in everyday menstrual products.
At last, that conversation reached one of the most powerful rooms in the country.
In October 2025, the House of Lords hosted “Have We Reached the Tipping Point for Toxic Period Products?”, part of Environmenstrual Week led by the Women’s Environmental Network (WEN).
Bringing together politicians, scientists, NGOs, and advocates, the event asked one central question: if the evidence is already clear, what’s stopping us from protecting people who menstruate?
The Political Will Is Growing, Slowly
Baroness Natalie Bennett, former Green Party leader and long-time environmental campaigner, opened the event with characteristic honesty: progress in Westminster is real, but painfully slow.
She spoke candidly about the challenges of turning concern into regulation.
“Politics is a process, not an event,” she reminded the room. Amendments fail, votes are lost, and yet each attempt builds pressure for change.
Her remarks reflected the growing cross-party awareness that chemical safety in menstrual products is a public health issue, not a niche concern.
In the UK, these products are still classified as consumer goods, unlike in the US, where they fall under medical devices.
That distinction matters; it shapes what’s tested, what’s disclosed, and ultimately how safe products are allowed to be.
A Four-Year Window for Change
Bennett called the current moment a “rare window of opportunity.” With Emma Hardy now serving as Secretary of State at the Department for Environment, Food and Rural Affairs , there’s a chance to align environmental, health, and equality goals, something that hasn’t happened before.
She urged everyone in the room to act decisively over the next four years, while the government is receptive and the public momentum is strong.
This is a political sweet spot: the science is mounting, public awareness is rising, and even large brands can see that consumer trust depends on transparency.
Her message was clear: don’t let this window close without action.
Regulations for period products could mirror those for cosmetics or drinking water, where safe thresholds are continually lowered as research reveals new risks.
From Stigma to Policy
Bennett also reflected on how far the conversation has come.
She recalled going on BBC Radio 4’s Women’s Hour in 2015 to talk about the tampon tax, when hearing party leaders say the word tampon on air was considered revolutionary.
A decade later, Westminster is not only saying the words but debating what’s inside those products.
For Bennett, normalising the language is part of dismantling the stigma. “Just use the words,” she said. “Put it out there.”
That cultural shift is as powerful as any policy change.
When menstruation is treated as a normal part of life, not a taboo, it becomes easier to discuss safety, sustainability, and rights — openly and without shame.
Coalition Building: The Real Engine of Progress
One of the most practical takeaways from the session was Bennett’s emphasis on coalition-building.
Regulation won’t happen through Parliament alone; it needs the force of public demand.
She pointed to the Women’s Institute, which has already campaigned for over a decade on microplastics, and encouraged collaboration with trade unions, community organisations, and campaign groups like WEN, PAN UK, and Natracare.
Her point was simple: the communities most affected by chemical exposure — lower-income groups, industrial workers, those living near polluted areas — are often least represented in policy rooms.
Building a coalition across environmental, feminist, and labour movements is how systemic change takes root.
Momentum, Awareness, and Responsibility
The House of Lords event marked a shift from awareness to accountability.
After years of grassroots activism and scientific evidence, from toxic metal testing to pesticide exposure studies, the discussion has finally reached the people who can make change possible.
For those of us in the menstrual equity movement, the message was energising. We’ve come a long way since the days when period poverty was barely discussed, let alone period safety.
But as Bennett reminded everyone, politics moves at a glacial pace, and every window of opportunity must be used wisely.
Change won’t come from Parliament alone.
It will come from pressure, from consumers, campaigners, and companies who believe that safe periods are a basic human right.
Learn more about WUKA at wuka.co.uk
Mental health
Acceptable data use vs exploitation when women receive ‘free’ digital health tools

By Wolfgang Hackl, CEO, OncoGenomX Inc., Allschwil, Switzerland
In women’s health, “free” digital tools occupy an especially sensitive space. Period trackers, fertility apps, pregnancy platforms, menopause programs, pelvic-floor wearables, contraception reminders, mental-health chatbots and symptom diaries have become essential resources for millions worldwide. For many, these tools fill longstanding gaps in clinical care, offering information, monitoring and community.
Yet women’s health data are uniquely intimate, politically vulnerable and commercially valuable. The same apps that help a woman identify a fertility window or track post-partum mood changes may also collect sexual history, location, device IDs, hormonal patterns, and behavioral clues that can be monetized or repurposed – sometimes without meaningful transparency.
The core ethical question is urgent: When does the data exchange that underpins “free” women’s health tools empower individuals, and when does it exploit them?
Across research and policy commentary, the fault lines remain the same – transparency, proportionality, control, fair value sharing, and protection from harm – but their stakes are heightened in women’s health.
The high-risk profile of women’s health data
The sensitivity of women’s health data is not abstract. It becomes dangerous in real-world contexts:
- Reproductive rights volatility – In jurisdictions with restrictive reproductive laws, menstrual cycle data, geolocation patterns around clinics, search histories and communication logs can be weaponized.
- Stigma and discrimination – Data related to miscarriage, abortion, infertility, menopause symptoms, mental health, sexual function or domestic violence can lead to insurance denial, unfair pricing, employment impacts or social vulnerability.
- Relationship and safety risk – Some apps collect or expose data that partners or third parties could misuse, from mood logs to location traces.
- Commercial targeting – Women are historically targeted with exploitative advertising around fertility supplements, weight loss, anti-aging and alternative therapies, often amplified by intimate behavioral data.
These risks transform the ethics of “free.” When a tool’s business model depends on collecting sensitive reproductive or behavioral attributes at scale, the user is no longer the beneficiary – the user is the product.
What women expect when sharing health data
Studies consistently show broad support among women for sharing data when it drives tangible health benefits—research, better care pathways, early diagnosis, or community insights. Trust collapses when data are:
- shared with advertisers, data brokers or insurers
- used for profiling, risk scoring or targeted pricing
- stored indefinitely or without clarity
- accessible to third parties unknown to the user
Women expect three things above all:
- Radical transparency
Not euphemisms, not hidden trackers, not 30-page terms. Women want to know who sees what, why and how it will be protected.
- Meaningful agency
Granular control – “yes” to sharing anonymized cycle data for research, “no” to targeted ads; “yes” to contributing to public-good datasets, “no” to third-party data inference.
- Safety guarantees
Technical and legal safeguards that explicitly prohibit uses exposing women to legal, financial, physical or psychological risk.
Women’s health is not a sandbox for broad, open-ended data collection. When platforms request permissions unrelated to their core health function – photos, contacts, continuous location, device fingerprinting – alarm bells ring.
Exploitation patterns in “free” women’s health tools
Technical audits of menstrual and fertility apps show that many collect extraordinarily detailed data: cycle length, symptoms, sexual activity, pregnancy intentions, test results, mood logs, sleep, stress, location, device IDs, email metadata, and “other information.” Some share with dozens of third parties.
The exploitation signals are increasingly well understood:
- Opaque data pipelines to marketers, analytics firms and profiling engines
- Unbounded storage of sensitive reproductive histories
- Engagement-driven design that nudges users toward disclosing more
- Commercial re-use of intimate behavioral patterns unrelated to health
- Minimal or performative governance despite high-risk categories
When a woman logs cramps or sexual activity, the ethical baseline is higher than in general wellness apps. The potential harms – legal, social, relational – are uniquely gendered and often irreversible.
Value capture and the “women pay twice” problem
Women’s health technologies have become a multi-billion-dollar market. But the value chain often flows upward, not back to the users:
- Women supply intimate, high-granularity data – Immense value for R&D, precision marketing, and investor storytelling.
- Companies monetize the insights – Through partnerships, advertising, risk scoring or AI model development.
- Women then purchase the resulting products – Including paid upgrades, supplements, or premium diagnostics whose innovation was subsidized by their data.
Without mechanisms that guarantee affordability, open reporting or reinvestment into women’s health services, the model becomes extractive. Women contribute the raw material, then buy back the finished product at retail price.
Pathways to acceptable – and truly empowering – data use
Responsible data practice in women’s health requires stricter standards than generic “digital health ethics.” The following markers – derived from current scholarship—are especially critical in women’s health contexts:
- Purpose-bound data practices
Tools should collect only what is strictly necessary for the health purpose. Fertility predictions do not require contact lists or persistent location tracking.
- Prohibitions on harmful secondary uses
Contracts and code must explicitly block:
- insurance scoring
- law enforcement access without due process
- targeted advertising linked to reproductive data
- cross-platform tracking
- sale to data brokers
- High-security architecture
Women’s health data should be treated like genomic or mental health data:
- encryption at rest and in transit
- zero-trust design
- independent security audits
- strict third-party access regimes
- Governance designed for vulnerable contexts
Oversight bodies should include women’s health experts, legal scholars, and patient advocates, reviewing not just privacy compliance but real-world harm potential.
- Fair value and reciprocity
If population-level reproductive or maternal health data fuel AI models, companies should commit to:
- affordability of products derived from those models
- investment in community health infrastructure
- transparency in data-driven improvements
This is not charity. It is ethical reciprocity.
The way forward: trust as a differentiator
Women’s health is evolving from niche to mainstream. With this visibility comes responsibility. Investors and innovators who treat data stewardship as a strategic asset – not a compliance hurdle—will define the next era of digital women’s health.
The future belongs to tools that:
- put safety ahead of scale
- align business models with women’s interests
- eliminate dark patterns
- prove that “free” does not mean “exploitative”
- create value with, not from, women
Ultimately, the line between acceptable data use and exploitation is shaped by one question:
Does this tool treat women as partners—or as data sources?
The companies that choose the former will earn the trust that defines the next generation of global women’s health innovation.
-

 Features2 weeks ago
Features2 weeks agoCannabis compounds kill ovarian cancer without harming healthy cells, research finds
-

 Opinion4 weeks ago
Opinion4 weeks agoFemtech in 2025: A year of acceleration, and what data signals for 2026
-

 Insight3 weeks ago
Insight3 weeks agoMeta removes dozens of abortion advice and queer advocacy accounts
-

 News4 weeks ago
News4 weeks agoRound up: First wearable detects symptoms of perimenopause, and more
-

 Mental health3 weeks ago
Mental health3 weeks agoSperm donor with cancer-causing gene fathered nearly 200 children across Europe
-

 Mental health4 weeks ago
Mental health4 weeks agoInsomnia combined with sleep apnea associated with worse memory in older women
-

 News3 weeks ago
News3 weeks agoUK couples exploiting legal loophole to rank embryos based on IQ, height and health
-

 Hormonal health4 weeks ago
Hormonal health4 weeks agoFemtech firm launches genetic test for perimenopause