News
California start-up raises US$1.5m to address maternal mental health problems
Mavida Health aims to make highly specialised, wrap-around care easily accessible and affordable for new and expectant mothers

California-based start-up Mavida Health has secured US$1.5m in pre-seed funding to address maternal mental health problems.
Mavida Health is a passion project founded by two women who have personally navigated the rollercoaster of motherhood.
The start-up, co-founded by Dr Sarah Oreck and Emma Sugerman, aims to address the growing concern of mental health disorders among new and expecting mothers and make highly specialised, wrap-around care easily accessible and affordable.
One in seven women who have experienced childbirth grapple with postpartum depression, yet nearly half of them remain untreated, according to recent research.
In the UK, as many as one in five women develop a mental illness during pregnancy or in the first year after birth. Despite this, many pregnant women and new mothers are left with no access to specialist community perinatal mental health services.
“Mavida Health is more than just a platform; it’s a lifeline for mothers everywhere,” says Dr Oreck, one of a handful of doctors with specialised training in reproductive psychiatry where she combines medical treatments with talk therapy, meditation, and a whole-body complementary approach.
“Unlike most existing solutions, Mavida Health adopts a holistic “whole village approach”to mental health, offering a comprehensive suite of services that range from personalised therapy to medication management, alongside a wealth of carefully curated content.”
The start-up has successfully raised US$1.5m in pre-seed funding led by Lakehouse Ventures, a seed stage venture capital firm that supports founders during the earliest days of business formation.
The company will use the funds to build its product, including the Mavida Health app, and build out its team as the start-up scale from launch to their next phase.
Hormonal health
Why period pain feels worse in winter

By Ruby Raut, founder and CEO, WUKA
If you have ever noticed that your cramps feel sharper, your mood dips harder, or your energy seems to disappear during the colder months, you are not imagining it. Winter can genuinely make periods feel more painful and more difficult to manage. The combination of cold weather, less sunlight, increased tension in the body, and reduced activity creates the perfect storm for stronger cramps and heavier emotional symptoms.
Understanding why this happens gives you the power to manage your cycle with more confidence. Here is the most digestible explanation of why winter and period pain are so closely linked.
Cold weather tightens blood vessels
When temperatures drop, your body goes into protection mode. To conserve heat, it tightens your blood vessels, especially around your hands, feet, and lower abdomen. While this is a smart survival response, it comes with an unwanted side effect for menstruation.
Your uterus is a muscle. Like any muscle, it needs good blood flow to relax and function smoothly. When the blood vessels around your pelvis tighten, circulation naturally becomes slower. Less blood flow means the uterus has to contract harder to shed its lining, and this can make cramps feel deeper, sharper, and more persistent.
This is why heat has always been one of the most effective comfort tools during a period. Warmth helps blood vessels open again, improves circulation, and relaxes the muscle of the uterus.
Your muscles tense up in the cold
Cold weather does more than chill your skin. It makes your whole body tighten without you even realising it. Think about how your shoulders creep upward when you step into the winter air or how your spine curls slightly for warmth. The same tension can build in your abdomen and pelvic floor.
Tighter muscles mean more resistance against the natural contractions of the uterus. When everything around the uterus is tense, cramps can feel more intense and more difficult to soothe. Even mild pain can feel magnified when the surrounding muscles are already stiff.
This is one of the reasons gentle movement, stretching, and warm baths can make such a difference during winter periods. Anything that eases tension also eases pain.
Less sunlight affects your mood and pain perception
Winter brings shorter days and longer nights, and that naturally reduces your exposure to sunlight. Sunlight plays a key role in regulating serotonin, the hormone that helps stabilise mood and influences how we experience pain.
Lower serotonin can lead to lower energy, stronger mood swings, and more emotional sensitivity. Because serotonin also impacts the way the brain processes discomfort, low levels can make cramps feel more intense.
This emotional shift can make PMS symptoms feel heavier too. Irritability, sadness, and bloating can all feel amplified during the colder months, creating a cycle that feels harder to manage.
Winter usually means less movement
Colder months naturally lead to less physical activity. We walk less, we spend more time indoors, and many people find it harder to stay motivated to exercise. While rest is important, the lack of movement has a direct impact on period pain.
Moving your body improves blood circulation and reduces inflammation. When you sit for longer or avoid movement due to cold weather, blood flow becomes slower and inflammation can rise. Both of these factors contribute to stronger cramps.
Even gentle activity makes a difference. A short stretch, a ten minute walk, or simple breathing exercises that open the chest and abdomen can support circulation and ease pain.
Prostaglandins may spike in colder weather
Prostaglandins are natural chemicals that help the uterus contract during menstruation. Higher levels are linked to stronger cramps and heavier flow. Some research suggests that colder temperatures and lower physical activity may increase the production of prostaglandins, although this varies from person to person.
This means that the natural winter slowdown combined with the physical effects of cold weather can lead to more intense uterine contractions, which again results in more painful periods.
How to make winter periods easier
The good news is that small, accessible habits can make a big difference to how your body feels during winter.
Use warmth generously
Heat patches, warm showers, hot water bottles and cosy clothing help open up blood vessels and soothe the uterine muscle.
Move your body even a little
Short walks, stretching routines or low impact workouts help improve circulation and reduce inflammation.
Support your mood with sunlight
Get outside during daylight hours whenever possible. Sitting near windows or using a light therapy lamp can also support serotonin levels.
Eat warming and nourishing foods
Soups, ginger, turmeric and herbal teas help comfort the body and may reduce inflammation.
Choose period products that keep you comfortable
Secure, breathable period underwear can help you feel more relaxed and confident, especially when your body already feels tense from the cold.
Winter does not have to mean more painful cycles.
With warmth, gentle movement, and an understanding of how your body responds to the season, you can navigate cold month periods with more comfort and control.
Find out more about WUKA at wuka.co.uk
Opinion
The hormone disruptors hiding in period products

By Ruby Raut, founder and CEO, WUKA
When we think of period products, the usual concerns are comfort, absorbency, cost and maybe sustainability. But there is another dimension — one less talked about but increasingly evidenced: chemical exposure via intimate-use products, and what this might mean for hormones, fertility, our microbiome and long-term health.
What Are Endocrine Disruptors?
Endocrine-disrupting chemicals (EDCs) are substances that either mimic, block or interfere with the body’s natural hormones. These hormones regulate growth, development, reproduction, metabolism and more. Exposures to EDCs have been linked to irregular periods, early puberty, infertility, PCOS (polycystic ovary syndrome) and endometriosis, among other conditions.
Although most public conversation about EDCs centres on plastics, food packaging, and household chemicals, this issue is now being traced into period products too.
Why Period Products Are a Unique Exposure Route
The route of exposure matters — and for period products it matters a lot. External products like pads or period underwear sit on the skin; yes, there’s absorption, but the skin provides more of a barrier than the internal mucosal tissues of the vagina and vulva. When products are inserted (tampons, menstrual cups) or used intimately against highly vascular mucous membranes, chemical absorption can be 10–80 times higher than skin contact.
This means that a small amount of a problematic chemical in a tampon or reusable underwear could result in a greater internal dose than a similar substance used externally. Moreover, because the vaginal route can bypass the liver’s first-pass metabolism, the body’s defences are fewer — increasing the potential for impact.
What Research Is Finding
Recent reviews of menstrual product testing reveal worrying patterns:
- A systematic review found that menstrual products (tampons, pads, liners) contained a variety of EDCs including phthalates, parabens, volatile organic compounds, dioxins and dioxin-like compounds.
- Studies of PFAS (per- and polyfluoroalkyl substances) — the so-called “forever chemicals” — show these synthetic compounds are endocrine disruptors and are increasingly linked to fertility challenges, PCOS, early puberty, and other hormone-mediated outcomes.
- For example, one S. study found higher PFAS levels among women seeking fertility treatment and a link to increased PCOS risk.
- Another study found that many reusable period products had high levels of PFAS, even though PFAS aren’t strictly necessary for functionality — meaning the exposures are avoidable.
What Does That Mean for You?
It’s tempting to read these findings and feel overwhelmed. Yes, we live in a chemically complex world — from pollution in the air to additives in food — but what makes this different is frequency of use, intimate contact, and cumulative exposure.
Think of it like this: someone might use a tampon (or other internal product) many times a month, for decades. The small dose of an EDC each time may be low, but over time it adds up — especially if it bypasses detox filters and steadily influences hormone networks.
That’s why brands and regulators need to shift from “Is there some chemical present?” to “What is the dose, for how long, by what route?” — and what that means for human biology over years.
Steps Towards Better Protection
- Ask about disclosure and testing: Brands should publish test reports and confirm they’ve checked for EDCs, PFAS, and reproductive-toxic chemicals.
- Prefer products without unnecessary chemical finishes: For instance, water-repellent or “antimicrobial” coatings may add PFAS or biocides; research shows many products function fine without them.
- Consider internal vs external product choices: While convenience and comfort matter, understanding how products are used helps you make informed decisions.
- Advocate for regulation: Science is building, and policies are starting to reflect the risk. But consumers’ voices help accelerate change.
WUKA’s Commitment
At WUKA we believe that transparency and rigorous testing aren’t optional — they are essential. That’s why we test every period underwear batch (in China and again in the UK via Eurofins) to ensure no PFAS are detected and no known reproductive-toxic chemicals are present. If I wouldn’t use it myself, I wouldn’t make it for anyone else.
Looking Ahead
There’s still much we don’t know: the exact doses absorbed through vaginal tissues, how mixtures of chemicals interact in the body, or the long-term impact of low-level exposures. But that’s all the more reason to act now rather than wait. EDCs affect not just one body, but generations.
In the end, it’s about more than fear — it’s about empowerment. Knowing what is in the products we use gives us the power to insist on better safety, better transparency and better health. Because safe periods aren’t a luxury, they’re a basic human right.
News
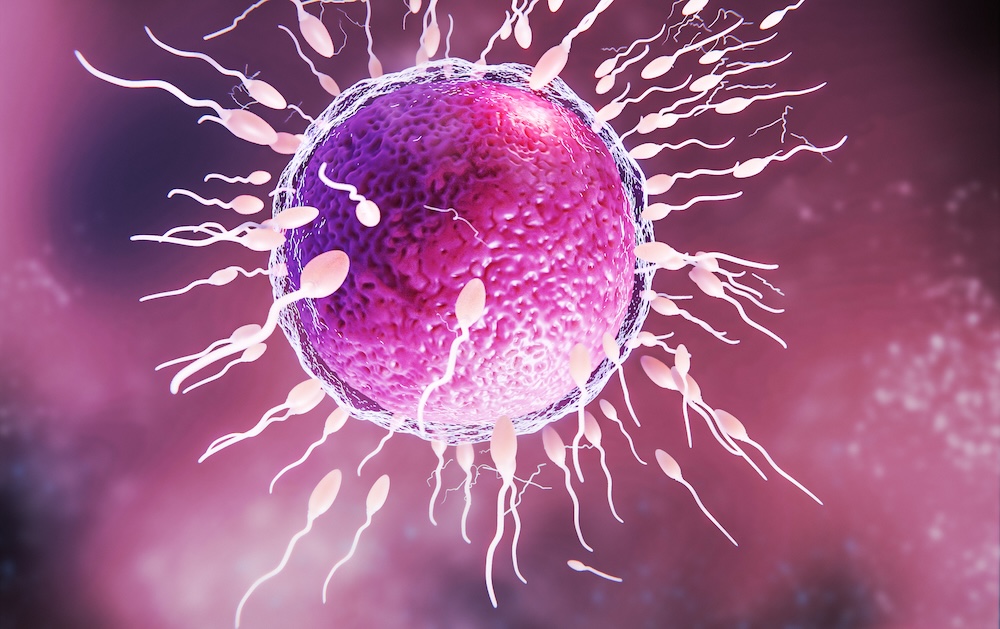
Can biotech help close the fertility gap? Inside the race to improve egg quality

With delayed parenthood now the norm, a new wave of biotech innovators is targeting the root cause of rising infertility rates. Oxford-based startup Uploid tells Femtech World how addressing egg ageing could reduce the “age penalty” that currently defines fertility outcomes.
Infertility now affects an estimated one in six people worldwide, with the World Health Organization determining it to be a “major public health issue.”
Across the OECD, the average age of first-time mothers has risen consistently over the past decades, driven by economic pressures, career progression, delayed partnership, and the availability of contraception. But human biology has not kept pace with this societal shift.
Egg quality declines sharply with age, beginning as early as the mid-thirties. It is this decline, not the body’s ability to carry a pregnancy, that remains the most significant factor behind falling conception rates.
IVF attempts to work around this challenge, yet even with technological advances, success rates remain modest. For women aged 18-34, birth rates per embryo transfer were around 35 per cent in 2022, dropping to five per cent by the age of 43-43.
“Fertility outcomes fall, not because the body is unable to sustain a pregnancy, but because egg quality declines with age,” Dr Alexandre Webster, co-founder and chief scientific officer at Oxford-based biotech firm, U-Ploid, tells Femtech World.
“Most existing fertility treatments are limited in how directly they can address this biological constraint. While IVF has advanced significantly in helping clinicians identify embryos with the best chance of success, there are currently very few options to intervene earlier and improve the quality of the eggs themselves.”
Current fertility treatments tend to focus on hormonal stimulation to produce more eggs, improving embryo selection, or improving implantation rates through uterine optimisation.
But none of these approaches address the root cause of age-related infertility, which is the egg’s declining ability to divide its chromosomes correctly.
This unmet need has set the stage for a new generation of reproductive biotech innovators, focusing on novel therapeutics, cellular engineering, AI-driven diagnostics, and biomarkers that could change how infertility is understood and treated.
A new frontier in fertility treatment
Among these innovators, U-Ploid is pioneering a new therapeutic category with Lyvanta™, a first-of-its-kind drug aimed at improving egg quality by addressing the biological mechanisms of maternal ageing.
Central to its approach is meiotic aneuploidy, which occurs when chromosomes fail to separate correctly as an egg matures. This increases dramatically with age, Webster explains, and is the leading cause of failed IVF cycles, miscarriage, and natural infertility. Studies have shown that over 50–80 per cent of embryos from women in their early 40s exhibit chromosomal abnormalities.
Lyvanta™ is designed to reduce the risk of these errors at the egg stage, before fertilisation occurs. It is injected into the egg before IVF, where it acts to stabilise chromosome segregation during meiosis.
“What makes this approach distinct is that, today, there are no approved or clinically available therapies that directly address meiotic aneuploidy or improve egg quality at its biological source,” Webster says.
“Lyvanta™ therefore represents a genuinely new therapeutic category. It does not act on embryos, does not alter DNA, and does not involve genetic modification. Instead, it supports a natural biological process that becomes increasingly error-prone with age.”
Evidence-gathering and regulatory engagement
The programme is grounded in over a decade of global academic research in chromosome biology and maternal ageing, and Uploid has carried out mechanistic studies, preclinical validation in aged animal models, and tightly regulated human egg studies in collaboration with IVF clinics.
However, the drug is still in the early stages of development, and the company is taking a cautious, evidence-driven approach.
Over the next one to two years, the research team will focus on building the scientific evidence needed to demonstrate clinical safety and efficacy. Meanwhile, regulatory engagement is ongoing, and timelines will depend on the outcomes of these studies.
“As with any new therapeutic, progress toward the clinic requires careful, stepwise evidence generation and regulatory review,” Webster says.
“Our focus at this stage is on ensuring that any future progress happens within established scientific, ethical, and regulatory frameworks. We engage with regulators, clinicians, and patient stakeholders to understand expectations around safety, evidence, transparency, and consent, and to ensure that the questions being asked of a new reproductive therapeutic are addressed rigorously and appropriately.”
He adds: “Lyvanta™ will only move forward if it meets the required standards set by regulators and ethics bodies, and only following thorough evaluation.”
If successful, the impact could be considerable. Improved egg quality may mean fewer IVF cycles, more viable embryos, and overall better outcomes for patients.
“If a therapy like Lyvanta™ can safely improve egg quality, it could lead to more viable embryos per IVF cycle, fewer cycles needed to achieve pregnancy, and better outcomes for people whose chances of success currently decline sharply with age,” Webster says.
“While much work remains, this is the long-term impact we are working toward.”
Global access and affordability
Globally, infertility affects people at similar rates regardless of income, but access to advanced treatments is often dependent on financial barriers.
IVF remains expensive worldwide. In the UK and US, a complete IVF cycle typically costs several thousand to tens of thousands of pounds, often requiring multiple attempts.
“One of the reasons fertility treatment is so costly and emotionally taxing is that patients often require multiple IVF cycles to achieve a successful outcome,” says Webster.
“Indeed, some 70 per cent of couples that start an IVF journey will end it with no baby, having run out of money and patience before a successful outcome.
By making each IVF cycle more efficient, it could reduce some of these costs and make treatment more accessible to more people.
“By improving egg quality upstream, Lyvanta™ has the potential to increase efficiency per cycle, which could reduce the overall burden, financial, physical, and emotional, on patients and healthcare systems,” Webster says.
The therapy is also being designed to integrate into existing IVF workflows, without requiring new infrastructure or highly specialised equipment.
He adds: “By focusing on improving biological efficiency rather than adding complexity, we believe this approach has the potential to support broader access over time, including in low- and middle-income countries where need is high but resources are limited.”
The new wave of fertility innovation
U-Ploid is part of a new wave of fertility biotech innovators. Companies such as Oxolife, developing a first-in-class oral drug to improve implantation; Gameto, engineering ovarian support cells to optimise IVF and egg freezing; and Genie Fertility, uncovering molecular biomarkers to personalise reproductive care, are all reshaping the field.
While progress in the fertility space has been incremental for decades, breakthroughs in chromosome biology, cell engineering, and molecular therapeutics are changing what might be possible.
This new generation of therapeutic innovation could improve outcomes and expand options for millions navigating delayed parenthood, and allow fertility science to catch up with the realities of modern life.
“Our aim is to reduce the biological ‘age penalty’ that currently defines fertility outcomes, so that success is less tightly coupled to chronological age,” Webster adds.
“If successful, this could allow more people to build families on timelines that reflect modern social and economic realities.”
-

 Features3 weeks ago
Features3 weeks agoCannabis compounds kill ovarian cancer without harming healthy cells, research finds
-

 Mental health3 weeks ago
Mental health3 weeks agoMeta removes dozens of abortion advice and queer advocacy accounts
-

 Insight3 weeks ago
Insight3 weeks agoSperm donor with cancer-causing gene fathered nearly 200 children across Europe
-

 Insight4 weeks ago
Insight4 weeks agoUK couples exploiting legal loophole to rank embryos based on IQ, height and health
-

 Insight4 weeks ago
Insight4 weeks agoPlanned birth at term reduces pre-eclampsia in high-risk women – study
-

 Entrepreneur4 weeks ago
Entrepreneur4 weeks agoMetri Bio raises US$5m for endo therapeutics
-

 Features3 weeks ago
Features3 weeks agoUniversity of Leeds IVF spinout raises £3.5m
-

 News2 weeks ago
News2 weeks agoCan biotech help close the fertility gap? Inside the race to improve egg quality

























