News
The femtech pioneers revolutionising contraception

Since the pill was invented in the 1960s, there has been little progress in the world of female contraception, and many of the methods currently on the market come with unwanted side effects. With the rise of femtech, however, comes renewed focus on providing contraceptive solutions that work for women.
When it comes to contraception, the options for women haven’t changed for decades. From the hormonal pill to the IUD implant, many come with unwanted side effects and are not suitable for everyone.
Furthermore, women’s healthcare, of which contraception is a key part, has historically been under-funded and under-researched.
It’s a market ripe for disruption and innovation, which is exactly what the new breed of femtech pioneers are doing.
Period tracking apps
Tech to track menstrual cycles and symptoms is popular with both those women who are planning to conceive and those who definitely aren’t.
While tracking cycle lengths and ovulation times can help women decode the best time to get pregnant, it can also help those women who want a less invasive method of contraception, without having to use hormones.
One such app is Clue, one of the earliest entrants into the period tracking space, with around 13 million people. The team behind the app are preparing to launch a digital contraceptive, which will use a statistical prediction of ovulation as a birth control tool. This will let users know when they are more likely to fall pregnant so they can use birth control or abstain.
In the same vein is Natural Cycles, billed as the world’s first and only CE and FDA approved hormone-free, digital contraception solution.
With 1.5 million registered users it has shown to be 93 per cent effective with typical use, which rose to 98 per cent with perfect use – a similar level to the Pill, with none of the side effects.
Home delivery
In the US, access to contraception can be difficult, especially in more rural areas; around 1.5 million American women live in a county without a single health centre offering the full range of methods.
And the problem was only exacerbated during the Covid-19 lockdowns.
During the pandemic, digital health practice Nurx experienced a surge in requests for at-home delivery of contraception, with a 50 per cent spike in birth control requests, and 40 per cent for emergency contraception.
Following an initial online consultation, the firm delivers most types of birth control, from pills, rings, shots, and patches. It also offers an overnight home delivery of the morning-after pill, an emergency contraceptive that can help reduce chances of pregnancy if taken within three days of unprotected sex.
The perfect match
There are nearly 250 types of contraception available, so it can be hard for women (and prescribers) to have the time to find the right one.
London-based femtech start-up Tuune’s research found that 85 per cent of women did not feel that their doctor spent enough time to find the best birth control for them, 52 per cent of women, globally, experience side effects from their birth control, and 43 per cent of women believe they have a hormone imbalance but can’t get a doctor to diagnose it.
These findings were the catalyst for its innovative product, which uses AI and biological testing to match women with the most suitable contraception for them.
A topical treatment
Away from apps and deliveries, merging technologies have also found a new way to prevent pregnancy, in what its founders say is the biggest revolution in contraception since the Pill.
Copenhagen-based start-up Cirqle Biomedical has developed mucus engineering as a new alternative to hormonal birth control.
The first product based on the technology, named OUI, aims to be as effective as the pill with minimal side effects. It works by using small biopolymers to reinforce the natural mucus barrier in the cervix to make it impenetrable to sperm, preventing it from passing through the cervix and fertilising an egg.
The biopolymer used is derived from either mushrooms or the shell of crustaceans and is known to be biodegradable, non-toxic and already used in other FDA-approved medical devices.
An animal study demonstrated 100 per cent effectiveness and the firm is looking to start human trials in the near future.
Review platform
Contraceptive side effects are common, yet often not talked about or highlighted by medics. The Lowdown, an online review platform for contraception, aims to change that and allow women to make an informed choice.
It was developed by Alice Pelton, who, after being prescribed the Pill at 16, suffered a decade of mood swings before she connected her emotional state with her medication.
By collecting huge amounts of data through user-generated feedback, the site also allows women to check any symptoms they may be experiencing against their method of contraception, and search for alternatives by connecting users with expert advice.
News
NHS health checks to include menopause questions for the first time

NHS health checks will include questions about menopause for the first time, a move ministers say could help up to five million women in England.
The Department of Health and Social Care said the new questions, to be developed over the coming months, could be introduced from 2026.
Adults aged 40 to 74 without long-term conditions are eligible for these free checks every five years.
The checks currently screen for heart and kidney disease, type 2 diabetes, dementia and stroke risks.
Adding menopause questions marks what health secretary Wes Streeting described as giving women “the visibility and support they have long been asking for.”
Streeting said: “Women have been suffering in silence for far too long.
“They are left to navigate menopause alone, with very little support – all because of an outdated health system that fails to acknowledge how serious it can be.
“No one should have to grit their teeth and just get on with what can be debilitating symptoms or be told that it’s simply part of life.”
Around three-quarters of women experience symptoms such as hot flushes, night sweats, depression and sleep problems.
One in four describe their symptoms as severe.
National Institute for Health and Care Excellence guidance recommends hormone replacement therapy (HRT) as the first-line treatment. HRT can also help maintain muscle strength and reduce the risk of osteoporosis, where bones become weak and brittle.
Despite this, many women say they are not listened to or offered adequate support.
Dr Sue Mann, NHS England’s national clinical director for women’s health, said: “By tailoring NHS health checks to include questions around menopause, we hope more women will get the support they need to manage their symptoms.”
Experts welcomed the move but cautioned that access inequalities remain.
Professor Ranee Thakar, president of the Royal College of Obstetricians and Gynaecologists, called it “fantastic news” that could help reduce stigma, but said implementation would be key.
“For this change to have maximum positive impact we’d like to see a real focus on ensuring women from diverse ethnic communities and socially deprived areas are supported to access health checks, and excellent menopause training for healthcare assistants providing them,” she said.
Kate Muir, author of Everything You Need to Know About the Menopause (But Were Too Afraid to Ask), said: “This is desperately needed, particularly to provide evidence-based information for women on the benefits of HRT. GPs’ appointments are a perfect way to get knowledge into all communities.
“We know from NHS statistics that 23 per cent of white menopausal women are on HRT, but only 5 per cent of black and 6 per cent of Asian women.
“This may open doors.”
Janet Lindsay, chief executive of Wellbeing of Women, added: “Women and people from marginalised communities are less likely to know about or attend these [health checks], and progress on menopause support cannot leave them behind.
“Healthcare professionals must work with grassroots organisations in these communities to ensure those facing additional barriers receive the tailored care they need.”
Mental health
Timing is everything: What AI need to learn about HRT and brain health
By Morgan Rose, CNM, WHNP-BC, and Dr Kudesia, triple board-certified in Reproductive Endocrinology & Infertility (REI), Obstetrics & Gynecology, and Lifestyle Medicine
The timing of when women start hormone replacement therapy (HRT) may matter more than we ever understood.
The “critical window” for starting HRT isn’t just relevant to brain health; timing has also been shown to shape cardiovascular outcomes.
Early analyses of the landmark WHI trial missed this nuance, including women long past menopause and obscuring benefits seen in those who begin therapy sooner.
Recent research presented at the American Neurological Association Annual Meeting found that women who began HRT within five years of menopause had a 32 per cent lower risk of developing Alzheimer’s disease.
Yet those who started HRT more than five years after menopause showed higher levels of tau proteins, a hallmark of Alzheimer’s, in their brains.
This “critical window” concept challenges the one-size-fits-all model of menopause care. It suggests that when we start HRT, it can be just as important as whether we start it.
Researchers at Mass General Brigham found similar patterns: women who began HRT near the onset of menopause did not show increased Alzheimer’s risk, while those who experienced early menopause with longer lifetime estrogen deprivation faced a higher risk overall.
Why Timing Matters
Women face roughly a 1 in 5 lifetime risk of Alzheimer’s disease, compared to 1 in 10 for men of the same age. The sharp drop in estrogen during menopause may help explain that gap.
Estrogen supports energy production, blood flow, and inflammation control in the brain functions that wane as levels decline.
The data suggest that initiating HRT earlier (around perimenopause or early menopause) may preserve some of these neuroprotective effects, while starting too late could heighten risk once neurodegenerative changes have already begun.
One meta-analysis showed that HRT begun soon after menopause reduced Alzheimer’s risk by over 40 per cent compared to non-users, while starting after age 60 doubled the risk.
These findings don’t make HRT a blanket prescription; they make it a precision intervention.
The Clinical Nuances AI Must Understand
If AI is going to support menopause care safely and intelligently, it needs to understand the reasons behind the actions.
1. Timing Is a Risk Modifier
“Time since menopause” is not just a demographic; it’s a clinical determinant.
AI systems must understand that the same therapy can carry opposite implications depending on when it’s initiated.
2. HRT Is Not Monolithic
There are multiple formulations, routes, and combinations.
For women who still have a uterus, adding progesterone helps protect the uterine lining and lowers the risk of endometrial cancer that can occur with estrogen-only therapy.
Topical estrogen, which has much lower absorption into the bloodstream, may be appropriate for perimenopausal women who are still having periods or postmenopausal women with a uterus who need targeted relief of vaginal or urinary symptoms.
For example:
- Estrogen-alone therapy can raise the risk of endometrial cancer and is typically not recommended for women with a uterus.
- Topical estrogen, with much lower systemic absorption, may be appropriate for perimenopausal women still having periods.
These distinctions must be explicitly encoded into AI frameworks to avoid oversimplified or unsafe recommendations.
3. Safety Requires Scope and Referral
Complex topics like HRT timing and neuroprotection should always prompt an automatic follow-up:
“Please consult a menopause specialist or clinician (such as one credentialed through the North American Menopause Society) to discuss the risks, benefits, and best options for you.”
AI logic must mirror how clinicians practice by inviting deeper discussion, not replacing it.
From Symptoms to Systems Thinking
We need to move beyond viewing menopause as a set of symptoms to manage, and instead see it as a neurological and metabolic inflection point in women’s lives.
That means:
- Bringing conversations about HRT earlier, during perimenopause, when neuroprotective benefits may still be possible.
- Designing AI systems that recognise context and chronology, not just keywords.
- Making personalised, evidence-based menopause guidance accessible to every woman by cutting through misinformation and connecting her to trusted care.
The Bigger Picture
For too long, women’s midlife health has been under-researched and under-resourced. The result is a data gap, which can quickly become a bias when encoded into AI.
If we want women’s health AI to truly care, it must be trained on data that understands the complexity of hormonal transitions, not just the vocabulary of them.
Because the difference between “now” and “five years from now” can determine whether a woman ages with clarity or confusion.
AI should know that.
And soon, it will.
Dr Kudesia is nationally recognised for her expertise in fertility awareness, lifestyle, and culinary approaches to reproductive health, and her advocacy for reproductive rights.
Diagnosis
Women better protected against early Parkinson’s neurodegeneration, study finds
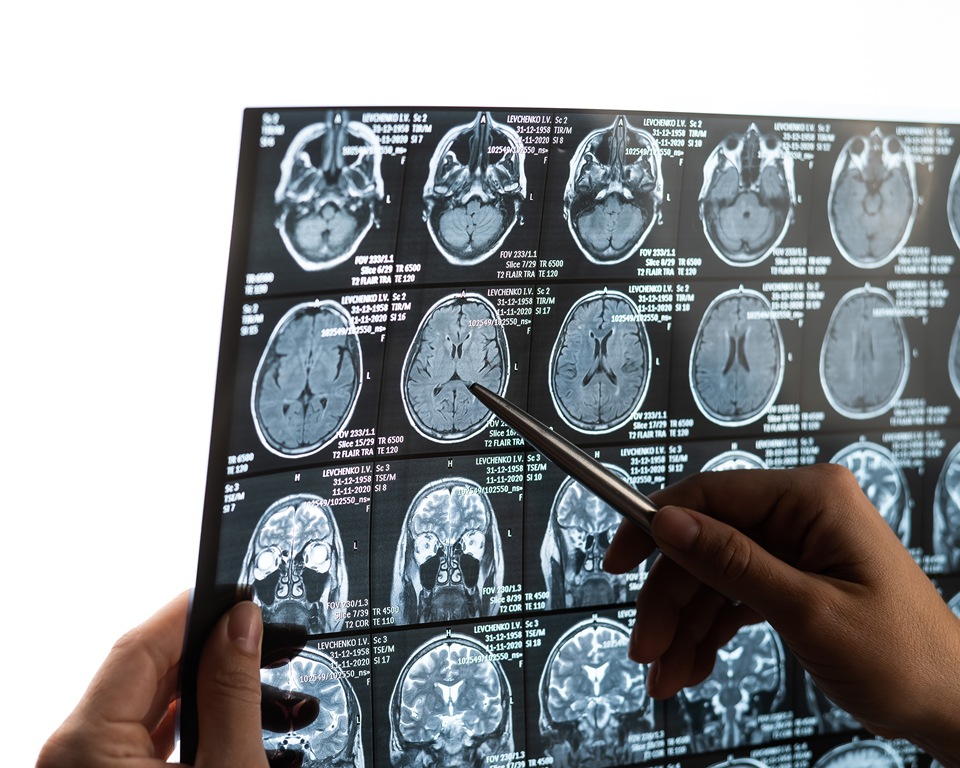
Women with an early precursor to Parkinson’s disease show much less brain shrinkage than men, despite similar disease severity, new research shows.
The discovery could help scientists explore how hormones might one day be used to treat the neurodegenerative condition.
The findings are based on data from nearly 700 participants across nine international research centres.
The study focused on isolated REM sleep behaviour disorder — a condition in which people physically act out their dreams.
It is considered the most reliable early warning sign of diseases caused by toxic protein build-up in the brain.
More than 70 per cent of those affected later develop Parkinson’s disease, Lewy body dementia or multiple system atrophy, which affects several body systems.
Researchers from Université de Montréal analysed 888 brain scans from centres in Canada, the Czech Republic, the UK, France, Australia, Denmark and Italy.
After quality checks, 687 participants were included: 343 patients with the sleep disorder and 344 healthy controls.
The results revealed clear sex-based differences.
While 37 per cent of the cortical areas — the brain’s outer layer responsible for higher functions — showed thinning in men, only one per cent of regions were affected in women.
This difference remained even though participants were of similar age (around 67) and had comparable clinical profiles.
Marie Filiatrault is first author of the study and a doctoral student at Université de Montréal.
The researcher said: “Men show much more extensive and severe cortical thinning — the outer layer of the brain that controls our higher functions — than women, particularly in areas linked to movement, sensation, vision and spatial orientation.”
To understand the protective effect, researchers compared brain images with gene activity in different regions, measured in healthy brains after death.
They found that the less-affected areas in women showed higher expression of genes related to oestrogen function, particularly ESRRG and ESRRA, which produce oestrogen-related hormone receptors.
The ESRRG gene was especially notable, showing greater activity in brain tissue than elsewhere in the body.
These receptors play key roles in mitochondrial function — the cell’s energy production system — and in the survival of dopamine-producing neurons, the cells that die in Parkinson’s disease.
Shady Rahayel is professor at Université de Montréal’s Faculty of Medicine and lead author of the study.
Rahayel said: “This sleep disorder offers a unique window of opportunity to study the mechanisms of neurodegeneration before major motor or cognitive symptoms appear.
“Our results suggest that certain brain areas in women with isolated REM sleep behaviour disorder are better protected than those in men, likely through the action of oestrogens.”
The team chose to study this precursor condition because it allows observation of brain protection mechanisms before major motor symptoms develop.
Although only 25 to 40 per cent of people with Parkinson’s experience REM sleep behaviour disorder, studying this early stage gives insight into how the brain resists damage when it is still limited.
Previous studies have shown that women with established Parkinson’s disease tend to experience slower progression than men, pointing to similar protective effects.
The findings could shape future research and treatment development.
The authors recommend separating men and women in clinical trials, which could improve statistical accuracy and reduce the number of participants required.
The biological mechanisms identified — particularly those linked to the ESRRG gene — could also become potential therapeutic targets.
Early laboratory research suggests that increasing ESRRG activity may protect dopamine-producing neurons from the toxic effects of alpha-synuclein, a protein that builds up abnormally in the brains of people with Parkinson’s.
“This study brings us closer to precision medicine, where treatments could be tailored not only to the disease but also to individual biological characteristics, including sex,” said Rahayel.

 News20 hours ago
News20 hours agoDozens of women report suffering painful burns after using Always sanitary towels

 News2 weeks ago
News2 weeks agoFDA plans to revise black box warning on menopause hormone therapies

 News2 weeks ago
News2 weeks agoAI-powered women’s health companion Nexus launches in UK

 News2 weeks ago
News2 weeks agoScientists turn human skin cells into eggs in IVF breakthrough

 Wellness7 days ago
Wellness7 days agoWomen’s health innovations recognised in TIME’s Best Inventions 2025

 Menopause2 weeks ago
Menopause2 weeks agoDaily pill could delay menopause ‘by years,’ study finds

 Insight2 weeks ago
Insight2 weeks agoAncient herb to modern must-have: Why ashwagandha is capturing UK women’s attention

 Menopause3 weeks ago
Menopause3 weeks agoNew report exposes perimenopause as biggest blind spot in women’s health


























5 Comments