Special
How to prepare for an egg freezing consultation
By Jenny Saft, CEO and co-founder of Apryl

Jenny Saft, co-founder of the fertility benefits platform Apryl, shares her tips on how to prepare for your first egg freezing consultation.
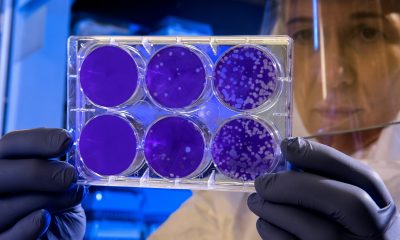
Egg freezing is a procedure that involves collecting a woman’s eggs from her ovaries and freezing them for use in the future.
There are a number of reasons why women may choose to freeze their eggs. Often, women want to preserve their fertility so that they can try and have a family when they are ready at a later date.
This is known as ‘social’ egg freezing. Women may also choose to freeze their eggs before undergoing medical treatment that may impact their fertility, such as chemotherapy. When a woman is ready to use the frozen eggs, they are defrosted and fertilised, before being transferred to the womb.
How to prepare for an egg freezing consultation
-
Research your clinic
Not all fertility clinics are created equal. So before selecting a clinic for your egg freezing procedure, it’s important to do your research.
Start by making a list of your priorities, such as cost, location or your connection with the fertility doctor. Also consider the areas where you might be willing to compromise. Once you’ve decided on your criteria for a clinic, you’ll be able to narrow down your options.
Comparing different clinics, visiting their facilities and reading reviews are excellent ways to obtain valuable information and build a bigger picture of the clinic before you commit.
-
Think through the questions you want to ask at your consultation
A fertility consultation can feel daunting. Preparing the questions you want to ask in advance can help you ensure you cover everything and don’t forget to ask about something that’s important to you.
A great question to ask (which people often forget) is ‘who are the clinic’s embryologists and how experienced are they?’. The quality of the embryologists will determine the quality of the egg freeze and thaw (should you eventually wish to use them).
Don’t be afraid to ask difficult questions and ask again if the answers you’re given aren’t clear.
-
Get clarity on costs
The exact cost of egg freezing procedures varies significantly from clinic to clinic – and will also vary depending on whether you eventually use the frozen samples, and how long they are in storage for.
Typically, one egg freezing cycle tends to cost between £3,800 to £5,000 in the UK, with an annual storage fee of up to £350. Sometimes, it can take women two or three cycles to collect the number of eggs they want to freeze.
There is no ‘perfect’ number, and the number of eggs you choose to freeze will depend on your age, ovarian reserves and reason for freezing. However, data does show that if you freeze at least 20 eggs before the age of 35, you have a 90 per cent chance of having at least one birth.
If you choose to fertilise the eggs and go for embryo transfer further down the line, this procedure can cost up to £5,000. So the whole process for egg freezing, thawing and transfer can cost anything up to £10,000, and sometimes more.
Getting clarity on estimated costs at the clinic you choose will help you to prepare financially and will prevent ‘surprise’ or unexpected costs from setting you back.
-
Check your workplace policy
Increasing numbers of employers are wrapping fertility support into their employee benefits packages. So, before you embark on your egg freezing journey, check what support is in place where you work.
From giving staff paid time off for consultations and treatment-related sickness, to actually funding fertility treatments themselves and supporting people with fertility counselling, there are lots of great ways employers are helping. If your company has a fertility benefits policy in place, use this to your advantage.
-
Mentally prepare for treatment side-effects
Egg freezing impacts different people’s bodies in different ways. Knowing about the potential side effects will help you to prepare for the ways in which your body might change.
For example, injecting yourself with medication to stimulate ovulation can feel difficult and invasive to begin with; and the drugs themselves can lead to side effects including bloating and mood swings.
The egg retrieval procedure can lead to cramps (similar, for many women, to bad period pains) and bruising around the abdomen. For most women, these side effects are more than worth it for the outcome. But if you know what to expect, you can be better prepared.
Overall, freezing your eggs should feel like an empowering experience and being prepared for your first consultation will help.
It’s important that you feel comfortable throughout the process, are able to trust your clinic and doctor and ask any questions that are on your mind.
News
Milken launches women’s health network platform
News
Innovate UK opens Women in Innovation Awards

Innovate UK has opened the Women in Innovation Awards for 2025 to 2026, with grants of up to £75,000 for as many as 60 winners.
HealthTech winners in 2024 included a tampon that prevents bacterial infections, an AI audio device for visually impaired people, and an app for gynaecological conditions.
The awards target female founders of late-stage start-ups with a minimum viable product, early user traction or revenue, growing teams and plans to raise significant capital within 12 to 24 months.
Liz Kendall, science secretary, said: “The Women in Innovation Awards are unlocking the UK’s untapped potential within our community of women innovators; if men and women started and scaled businesses at the same rate this could be worth as much as £250 billion for the UK economy.
“This record £4.5 million investment will empower ambitious women founders to scale their businesses, drive economic growth, and inspire the next generation of innovators.”
Applicants must operate in advanced manufacturing, digital and technologies, or life sciences, three of the high growth sectors identified in the UK’s Industrial Strategy. Winners receive up to £75,000 plus training, networking and role-modelling opportunities, with tailored support also offered to highly commended applicants.
The competition opened on 26 November 2025 and closes on 4 February 2026.
Since 2016, Innovate UK has invested more than £11m in 200 women innovators through these awards, with up to 60 more to be funded this year.
Last year’s programme drew criticism after Innovate UK initially said it would fund 50 women, then announced only 25 awards at £75,000 each. Following a campaign led by Emma Jarvis, founder of Dearbump, and the ‘Let’s Fund More Women’ group of more than 400 supporters, Innovate UK reversed the decision and confirmed all 50 awards and £4m, saying it was “a mistake and we prioritised wrongly”.
News
CardMedic and LanguageLine announce app integration

CardMedic, the digital platform transforming clinician and patient communication, has announced a major integration with LanguageLine Solutions, the global leader in on-demand interpretation.
The partnership brings one-click access to live, professional video and audio interpreters in more than 240 languages directly within the CardMedic app.
The integration will help clinicians deliver safe, inclusive, and human-centered care at the point of need.
Dr Rachael Grimaldi, co-founder and chief medical officer of CardMedic said: “Our mission is to remove barriers that stand in the way of safe, compassionate care.
“This integration with LanguageLine gives clinicians fast and reliable access to professional interpreters alongside all of CardMedic’s inclusive tools, making communication more effective and equitable than ever before.”
CardMedic’s digital app breaks down language, cognitive, and sensory barriers, providing clinicians with instant access to multilingual and multimodal tools that support patients across a wide range of communication requirements.
With LanguageLine’s trusted interpreter network now embedded into the platform, CardMedic becomes the only solution of its kind to combine prewritten clinical content, AI powered accessibility tools, and live interpretation in one seamless workflow.
CardMedic was quickly developed during the COVID 19 pandemic in response to urgent communication breakdowns caused by masks and PPE.
Since then, it has grown into a comprehensive healthcare language support platform, used across NHS trusts in the UK and expanding internationally into the United States.
Designed in collaboration with clinicians and refined through real patient feedback, the app is simple to use, fast to deploy, and built to fit within clinical workflows across acute, emergency, and routine care.
With the new integration, healthcare staff can connect to a live LanguageLine interpreter within seconds, directly inside the CardMedic app.
Whether a conversation starts with a multilingual script or with an AI powered sign language avatar, clinicians can now escalate immediately to human interpretation with no disruption to care.
The experience includes intelligent language selection, optional department code support, and device flexibility.
Early feedback from NHS and US health systems points to faster decision making, improved patient understanding, and reduced delays.
CardMedic’s AI is guided by a clinician in the loop model that ensures all content is accurate, culturally sensitive, and accessible at a 6 to 8-year reading level. The platform complies with GDPR, is tested to minimise bias, and is designed to complement human interpreters rather than replace them.
The result is a flexible, ethical, and scalable communication solution that strengthens understanding, safety, and trust across diverse patient populations.
CardMedic has been cited in NHS England’s 2025 Patient Safety Healthcare Inequalities Reduction Framework and supported by key innovation programs including the NHS Innovation Accelerator, Clinical Entrepreneur Programme, MassChallenge, and Texas Medical Center Innovation.
As healthcare systems continue to focus on reducing disparities, CardMedic’s all in one platform is uniquely positioned to support scalable, equitable care across urgent and planned settings.
Simon Yoxon-Grant, president and CEO of LanguageLine Solutions said: “When a clinician can connect with a patient in their own language, it affirms the patient’s right to be heard.
“We’re proud to work with CardMedic to deliver that kind of access at the point of care.”
Looking ahead, CardMedic is developing personalised interpretation pathways, digital consent support, and communication tools for underserved communities.
-

 Features2 weeks ago
Features2 weeks agoCannabis compounds kill ovarian cancer without harming healthy cells, research finds
-

 Opinion4 weeks ago
Opinion4 weeks agoFemtech in 2025: A year of acceleration, and what data signals for 2026
-

 Insight3 weeks ago
Insight3 weeks agoMeta removes dozens of abortion advice and queer advocacy accounts
-

 Menopause4 weeks ago
Menopause4 weeks agoRound up: First wearable detects symptoms of perimenopause, and more
-

 Insight3 weeks ago
Insight3 weeks agoSperm donor with cancer-causing gene fathered nearly 200 children across Europe
-

 Mental health4 weeks ago
Mental health4 weeks agoInsomnia combined with sleep apnea associated with worse memory in older women
-

 News3 weeks ago
News3 weeks agoUK couples exploiting legal loophole to rank embryos based on IQ, height and health
-

 Insight4 weeks ago
Insight4 weeks agoPlanned birth at term reduces pre-eclampsia in high-risk women – study


























Pingback: Fertility care is a necessity, not a luxury: how fintech can pave accessible pathways to parenthood - FemTech World
Pingback: Ivy Fertility acquires California-based fertility practice - FemTech World
Pingback: Record numbers of women are freezing their eggs, data shows - FemTech World
Pingback: New service to allow women with cancer in Hong Kong to preserve ovarian tissue - FemTech World