News
Australian scientists make world-first endometriosis treatment breakthrough
The findings could help researchers determine whether a woman will need fertility treatment
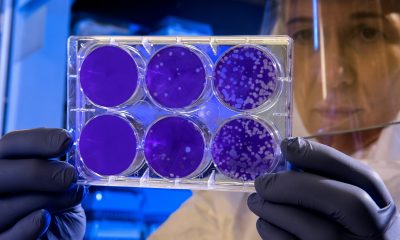
A team of Australian researchers has become the first in the world to grow tissue from every known type of endometriosis, in a move that could pave the way for new research into more effective treatments and diagnoses.
Researchers from the Royal Hospital for Women, Sydney will be able to test treatments and match patients’ symptoms with specific proteins, after successfully growing 30 different lab-grown tissues taken during surgery.
The advancement will not only allow scientists to vary treatments from different types of endometriosis, but it will also help them determine whether a woman will need fertility treatment in the future.
Endometriosis is a common disease where tissue similar to the lining of the womb grows outside it in other parts of the body.
According to Endometriosis Australia, more than 830,000 of Australian girls and women live with endometriosis at some point in their life, with the disease often starting in teenagers. However, symptoms can vary dramatically between patients.
The charity estimates the illness costs the country AUS$9.7bn per year, with AUS$2.5bn coming in direct healthcare costs, and the rest in lost productivity.
Professor of obstetrics and gynaecology at Sydney Royal Hospital for Women, Jason Abbott, said collecting the cells in one place for the first time would allow researchers to accurately diagnose patients, potentially limiting the need for invasive and painful surgeries.
“Very much like we thought breast cancer, 30 years ago, was one disease and treated in one way, we now understand that [endometriosis] is much more complex than that,” he told Brisbane Times.
“All those different types of endometriosis really probably reflect different diseases … and that [can determine] their response to treatment, clinical symptoms and also things like infertility.”
The development, Abbott said, would help fast-track new treatments by enabling researchers to test new and existing drugs on the lab tissues rather than in humans.
“It’ll mean that we’ll be offering new treatments just around the corner,” he added.
Endometriosis has often been referred to as the ‘missed disease’ due to its unclear aetiology and inconsistencies in its diagnosis and management.
Unlike other long-term conditions such as diabetes and asthma, reports suggest endometriosis has remained largely ignored in government policy and research funding globally.
A 2021 study concluded that while social science and feminist research has drawn attention to the historical absences around endometriosis and the exclusion of women’s accounts, more empirical work which explores the active construction of ignorance around endometriosis in contemporary healthcare and policy contexts is urgently needed.
Opinion
The science behind the scar: What’s really in our period products

By Ruby Raut, founder and CEO, WUKA
Over the past year, headlines about “toxic period products” have been hard to ignore. Stories about PFAS, heavy metals, and hormone disruptors in pads, tampons, and underwear have sparked global concern, and for good reason. But behind the fear, there’s a scientific story worth understanding.
At the recent House of Lords event, “Have We Reached the Tipping Point for Toxic Period Products?”, researchers and policymakers came together to separate fact from panic. The truth is more nuanced: yes, chemicals and metals are present in some menstrual products, but understanding how much, where they come from, and what that means for our health is key to driving change that’s informed, not sensational.
What Scientists Have Found So Far
Dr Kathrin Schilling, an environmental health scientist at Columbia University, shared new research that tested 16 metals in menstrual products, including arsenic, cadmium, lead, and antimony, all known toxic substances linked to long-term health effects such as cardiovascular disease, kidney problems, and hormonal disruption.
The findings were striking:
- Non-organic products showed higher levels of lead and cadmium than organic ones.
- Some reusable and single-use products exceeded 30,000 nanograms per gram (ng/g) of antimony, a toxic metal commonly used in plastics manufacturing.
- Lead levels varied dramatically, some products contained 100× more than others.
To put this in perspective, even very small doses of lead can cause harm. The World Health Organization confirms there is no safe level of lead exposure. Chronic, low-level contact can gradually affect the nervous system and fertility. The same applies to arsenic, where countries have tightened drinking water limits from 10 µg/L to as low as 1 µg/L after learning that long-term exposure causes disease.
So while the numbers in menstrual products might sound tiny, what matters most is frequency and route of exposure. Menstrual products are used regularly and in contact with one of the body’s most absorbent tissues — the vaginal wall — where absorption is estimated to be 10–80× higher than through skin. Over decades of use, even low concentrations can add up.
Understanding PFAS — The “Forever Chemicals”
Alongside metals, PFAS (per- and polyfluoroalkyl substances) have become another major concern. These synthetic compounds are used for absorbency and stain resistance — but they don’t break down easily, earning the name “forever chemicals.”
They accumulate in soil, water, and the human body, and have been linked to reproductive issues, thyroid disease, and immune dysfunction. California recently became the first state to ban PFAS in menstrual products, while New York is pushing for broader restrictions that include heavy metals and hormone disruptors.
These international shifts signal a clear message: the world is moving towards stricter, transparency-first regulation — something the UK could soon follow.
Why It Matters for Our Bodies
It’s important to remember that our world is already filled with background exposure, from air pollution, processed food, and household plastics. We all live in a chemically complex environment. The key isn’t to fear every product but to understand which exposures matter most and how to minimise them.
Menstrual products are unique because of their intimate and repeated contact with the body. Even trace chemicals can bypass the body’s natural detox systems when absorbed vaginally. This doesn’t mean every product is dangerous, but it underscores why regular, independent testing and clear ingredient disclosure are essential.
Internal vs. External Exposure: Why It Makes a Difference
One of the least understood parts of this debate is the difference between internal and external products. A pad or period underwear sits on the skin; it can only transfer chemicals through surface contact. But products like tampons or menstrual cups are inserted directly into the vagina, an environment that absorbs substances 10–80 times more efficiently than normal skin.
That’s because the vaginal wall is highly vascular, full of small blood vessels, and it bypasses the liver, the organ that usually filters and detoxifies harmful substances. So when a chemical is absorbed vaginally, it goes straight into the bloodstream.
Yet, most testing and regulation still treat all menstrual products as if exposure happens through skin contact. There’s very little research separating the risk profiles of internal (tampons, cups, discs) versus external (pads, underwear) products. That’s why scientists like Dr Schilling emphasised the need for new safety standards that actually reflect how the body interacts with these materials, not just how a fabric performs in a laboratory test.
How Responsible Brands Are Responding
Some brands are already ahead of regulation.
At WUKA, we take this responsibility seriously. We are one of the very few period underwear brands with no PFAS detected in our products. Every batch is tested rigorously, both at source (in China) and again in the UK by Eurofins laboratories, an independent global testing agency.
We also screen for toxic chemicals, metals, and harmful finishes, ensuring that what touches your body is as safe as it is sustainable. As a founder, I always remind our team: I use our products myself. If I wouldn’t wear it, I wouldn’t make it for anyone else.
Our philosophy is simple, transparency builds trust. Consumers shouldn’t need a chemistry degree to choose a safe period product.
The Path Ahead
The science is clear: menstrual product safety deserves the same rigour as drinking water, cosmetics, or food. But we can also take heart, awareness is growing, data is expanding, and governments are beginning to act.
As policymakers push for international standards (through bodies like the ISO TC338 on menstrual products), and as responsible brands lead by example, the future of menstrual care looks safer, smarter, and far more transparent than the past.
This isn’t just about fear of toxins, it’s about empowering everyone who menstruates with knowledge and choice. Because understanding the science is the first step toward changing it.
Find out more about WUKA at wuka.co.uk
Insight
Women face worse stroke recovery than men in first year, study finds
Insight
Caesarean births overtake natural vaginal deliveries in England for first time

Caesarean births (surgical births) have overtaken vaginal deliveries in England for the first time, with 45 per cent of births now by caesarean, NHS data show.
Last year, 44 per cent of births were through natural vaginal deliveries and 11 per cent were assisted with instruments such as forceps or ventouse, according to data published on Tuesday covering April 2024 to March 2025. Assisted deliveries use instruments to help the baby out during birth.
More than four in ten caesareans carried out by NHS England were elective, planned operations. For women under 30, natural vaginal birth remained the most common method, while for women aged 30 and over, caesareans were most common. For women aged 40 and over, 59 per cent of births were by caesarean.
In total, 20 per cent of births in 2024-25 were planned caesareans and 25.1 per cent were emergency, with both figures at record highs.
There were 542,235 deliveries in NHS England hospitals during this period, down from 636,643 in 2014-15. One in four births were to mothers aged over 35.
In 2014-15, caesarean deliveries made up 26.5 per cent of births. The increase over the past decade has been attributed to growing numbers of complex pregnancies, linked to factors including rising obesity rates and women waiting until they are older to have children.
Donna Ockenden, one of the UK’s most senior midwives who is leading the inquiry into maternity failures in Nottingham, told BBC Radio 4’s Today programme that the rise was a “complex” and “evolving picture over time”.
She said: “The thousands of women I’ve spoken to want a safe birth above everything else, so we should not vilify or criticise women who make those decisions.”
“In the reality of today’s maternity services – where women are living in poverty, deprivation, they’ve got pre-existing illnesses – obstetricians, midwives, nurses can only do so much, and we don’t always do enough in all cases to optimise women’s health prior to pregnancy.”
Soo Downe, a professor of midwifery at the University of Lancashire, added: “In some cases women are going for caesarean sections as a kind of least-worst option because they don’t really believe they’re going to have the kind of support they need to have a safe, straightforward, positive labour and birth in hospital.
“Or because their birth centres are being closed … or because they go into labour wanting a home birth and the midwife isn’t able to come to them because the midwife’s called somewhere else.
“But for some of them, it becomes the only choice on the table … and for other women, they choose a caesarean because they really want one, and that’s absolutely fine.”
-

 Features1 week ago
Features1 week agoCannabis compounds kill ovarian cancer without harming healthy cells, research finds
-

 Opinion3 weeks ago
Opinion3 weeks agoFemtech in 2025: A year of acceleration, and what data signals for 2026
-

 News4 weeks ago
News4 weeks agoInnovate UK relaunches £4.5m women founders programme
-

 Opinion4 weeks ago
Opinion4 weeks agoDoctors push back on ‘data-free’ ruling on menopause hormone therapy
-

 Insight2 weeks ago
Insight2 weeks agoMeta removes dozens of abortion advice and queer advocacy accounts
-

 Opinion4 weeks ago
Opinion4 weeks agoWhy women’s health tech is crucial in bridging the gender health gap
-

 Menopause3 weeks ago
Menopause3 weeks agoRound up: First wearable detects symptoms of perimenopause, and more
-

 Insight2 weeks ago
Insight2 weeks agoSperm donor with cancer-causing gene fathered nearly 200 children across Europe

























1 Comment