Fertility
Platelet-rich plasma may support ovarian function, could increase IVF success rates

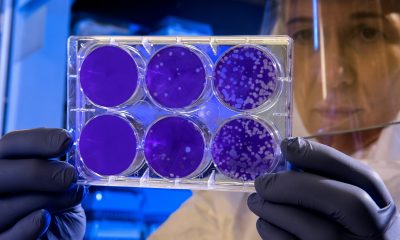
Researchers have found that a treatment called platelet-rich plasma (PRP) might help women with poor ovarian response, suggesting that PRP may enhance ovarian rejuvenation and improve egg quality, potentially increasing pregnancy success rates for women undergoing in vitro fertilization (IVF).
Diminished ovarian reserve is a major challenge in fertility treatments, affecting many women undergoing IVF.
It is associated with fewer collected eggs and lower pregnancy success rates. Some studies have explored PRP, a concentration of growth factors derived from a patient’s own blood, as a potential treatment to rejuvenate ovarian function. However, the biological effects of PRP treatment at the molecular level remain unclear.
In this study, the research team specialised cells that surround the egg, using RNA sequencing technology. Samples were collected from women aged 18 to 37 with poor ovarian response, who either received PRP therapy or standard treatment before IVF.
The results showed significant differences in gene expression between the two groups. PRP-treated samples exhibited increased activity in genes related to metabolism, cell survival, and communication between cells, all of which are crucial for egg development and fertility.
One key finding was that PRP influenced carbohydrate metabolism in cumulus cells.
This is essential, as cumulus cells provide energy to the developing egg, and previous research has linked metabolic health to embryo quality. PRP also appeared to regulate pathways related to cell proliferation and programmed cell death, suggesting it may help support egg survival.
Although PRP has been used in medicine for wound healing and tissue repair, its role in fertility treatment is still under investigation. Some clinical trials have shown improved ovarian reserve markers after PRP treatment, while others have not found a direct benefit for pregnancy rates.
This study sheds light on how PRP affects cumulus cells, offering valuable insights into its potential for improving fertility treatments.
The researchers, from IVIRMA New Jersey, Yale School of Medicine, Yale University, and Acibadem Mehmet Ali Aydinlar University, hope that further studies will help refine PRP treatments, determine the best protocols, and identify which patients may benefit the most.
By understanding the molecular effects of PRP on ovarian cells, scientists may develop targeted fertility therapies to support women facing infertility due to diminished ovarian reserve.
Insight
IVFmicro raises £3.5m to boost IVF success

IVFmicro has raised £3.5m to advance its microfluidic device designed to improve IVF success rates in routine clinic use.
The Leeds-based spinout from the University of Leeds, founded in 2024, aims to increase the quality and number of embryos in an IVF cycle.
IVF, or in vitro fertilisation, combines eggs and sperm in a lab before transferring embryos to the womb. A microfluidic device is a chip with tiny channels that move very small volumes of fluid.
The company says its device could raise the number of viable embryos available for transfer and the likelihood that an embryo will implant.
Currently, IVF leads to a successful pregnancy in about 30 per cent of cases for women under 35. A single cycle typically costs around £5,000 in the UK.
“My career has focused on understanding the reproductive biology of eggs and embryos, how they develop and, crucially, why things sometimes go wrong,” said IVFmicro co-founder and scientific director Helen Picton.
“At IVFmicro, we are harnessing years of research into reproductive biology to create a practical, accessible solution that can improve outcomes for patients undergoing fertility treatment. Our goal is to make IVF more effective, more predictable, and ultimately more hopeful for those striving to start a family.”
The investment was led by Northern Gritstone, with support from Innovate UK’s Investment Partnership Programme.
“IVFMicro is a brilliant example of the world-class innovation emerging from the Northern Arc’s universities, combining scientific excellence with a clear commercial vision to tackle the societal challenge of infertility,” said Northern Gritstone chief executive Duncan Johnson.
“Millions worldwide require fertility treatment, but new solutions are needed to overcome the high costs involved and low success rates. We are especially proud that IVFMicro’s journey has been supported through our NG Studios programme and our Innovation Services, which exist to help founders like Virginia and Helen turn pioneering research into real-world impact.”
Features
University of Leeds IVF spinout raises £3.5m

University of Leeds IVF spinout IVFmicro has raised £3.5m in pre-seed funding.
The investment is led by Northern Gritstone, with support from Innovate UK Investor Partnerships Programme, and will be used by IVFmicro for its next verification and validation phase, leading to trials on human embryos in fertility clinics.
Helen Picton is scientific director and co-founder of IVFmicro.
She said: “My career has focused on understanding the reproductive biology of eggs and embryos, how they develop and, crucially, why things sometimes go wrong.
“At IVFmicro, we are harnessing years of research into reproductive biology to create a practical, accessible solution that can improve outcomes for patients undergoing fertility treatment.
“Our goal is to make IVF more effective, more predictable, and ultimately more hopeful for those striving to start a family.”
Globally, 1 in 6 couples will face fertility issues, yet IVF success rates are suboptimal, with only 25-30 per cent succeeding in women under 35 years of age.
This is due in part to limitations of the embryo culture process, which typically involves repetitive handling, subjective selection of the best embryo, and the expense of highly skilled operators.
IVF is an expensive process, costing on average £5,000 for a patient in the UK for one cycle, accompanied by long NHS waiting lists that have selective criteria.
IVFmicro provides the first microfluidic device (a device for safely managing embryo culture and handling with very small amounts of nutrient-rich fluid) that can be used in any IVF treatment cycle.
This precision-engineered solution improves both the number of viable embryos available for transfer and the likelihood that an embryo will implant and result in a pregnancy.
IVFmicro provides a 10-15 per cent improvement in embryo quality and quantity, a significant leap that increases the potential to fall pregnant.
IVFmicro was founded in 2018 by Virginia Pensabene, Ph.D, and Helen Picton, Bsc, Ph.D., both professors at the University of Leeds.
Pensabene has published scientific advancements in microfluidics and brings her technical and scientific expertise to the product design.
Picton is a non-clinical expert in female reproductive biology and embryology, and has generated over £8m in research grant income.
IVFmicro recently took part in the NG Studios life sciences programme, which supports pre-seed life science businesses, and is delivered by accelerator KQ Labs, the Francis Crick Institute, and Northern Gritstone.
Virginia Pensabene, CEO and co-founder, IVFmicro, said: “As a biomedical engineer, I began exploring the potential of this technology in 2017, when Helen and I first met at the University of Leeds.
“From the start, our goal was to translate our research into a real solution for patients.
“Thanks to the combination of grant funding and Northern Gritstone’s support — both through investment and its innovation programmes — we have been able to grow our team in Leeds and take a major step toward bringing this precision-engineered IVF solution to market.”
Fertility
Meta removes dozens of abortion advice and queer advocacy accounts
-

 Features1 week ago
Features1 week agoCannabis compounds kill ovarian cancer without harming healthy cells, research finds
-

 Opinion3 weeks ago
Opinion3 weeks agoFemtech in 2025: A year of acceleration, and what data signals for 2026
-

 News4 weeks ago
News4 weeks agoInnovate UK relaunches £4.5m women founders programme
-

 News4 weeks ago
News4 weeks agoDoctors push back on ‘data-free’ ruling on menopause hormone therapy
-

 Fertility2 weeks ago
Fertility2 weeks agoMeta removes dozens of abortion advice and queer advocacy accounts
-

 Menopause4 weeks ago
Menopause4 weeks agoWhy women’s health tech is crucial in bridging the gender health gap
-

 Fertility3 weeks ago
Fertility3 weeks agoRound up: First wearable detects symptoms of perimenopause, and more
-

 Fertility2 weeks ago
Fertility2 weeks agoSperm donor with cancer-causing gene fathered nearly 200 children across Europe