Insight
‘Femtech addresses critical unmet needs in the women’s health space’

Dr Pamela Walker tells FemTech World everything we need to know about the femtech market.
Can you tell our readers a little bit about yourself?
I am a healthcare strategic growth specialist and award winning MedTech angel investor. I have been passionate about the healthcare space my whole life, and this drive pushed me to complete a PhD in Neuroscience, followed more recently by an Executive MBA (both from Oxford).
I have devoted my career to helping get treatments and medical devices to the patients that need them, and optimising the support patients, caregivers and healthcare professionals need to improve outcomes.
To make this impact, I work with Pharma and MedTech corporates as well as Private Equity and VC funds, advising on acquisitions and optimising commercialisations in the UK, US and worldwide. I am a Partner at Gate One, heading up the Life Sciences sector, Gate One Incubator and investment channel. I am also an avid investor with THENA Capital and Angel Academe, and board advisor to a number of our portfolio investments.
Why is it important to invest in femtech?
Femtech is an important sector, addressing critical unmet needs in the women’s health space. It leverages tech innovations that we have at our fingertips and applies them to critical gaps in healthcare for over 50 per cent of the world’s population.
In 2021, the gender healthcare gap gained visibility in the UK with the publication of the House of Lords Library report. This report highlights that the UK has the largest female health gap in the G20 and the 12th largest globally. This past summer, NHS England published its strategy on how the gap should be addressed.
Independent reports and inquiries have highlighted where this gap is most visible:
- Mental health, heart conditions, and pain treatment are some of the areas for which women are not offered the same level of care as men.
- Women’s health is under researched and is given a lower priority when it comes to health services: less is known about conditions that only affect women including common gynaecological conditions that can have severe impacts on health and wellbeing. For example, it takes seven to eight years for women to receive a diagnosis of endometriosis, with 40% of women needing 10 or more GP appointments before being referred to a specialist.
- Clinical research in women is dramatically lower than in men, and gender biases in clinical trials are contributing to worse health outcomes for women vs men.
This evidence has highlighted the need for greater focus on women’s health. The market must consider women as a sizeable consumer group. This is an underserved group that is increasingly educated, employed, and receiving attention from diversity and inclusion benchmarks at a global level.
Women represent an important consumer group to be marketed to and a discerning group that will prefer products relevant for them. Companies that consider them will win.
What do you think is missing in the femtech industry?
There are a number of novelty products and me-too solutions in this space, at the moment. Although there are products targeting key points in the female lifecycle, most, however, are still finding their feet. Some are missing a business model for longevity, others are very niche and will struggle to gain uptake, others have unclear value propositions. Overall, evidence of impact hasn’t quite yet pulled through, but there is a lot of excellent innovation kicking off.
From a product development standpoint, design and execution support is needed. There is a medium-term gap to address the gender healthcare gap imbalance through the drug and medical product development process. Innovations that optimise the development process with a gender balanced lens will be in demand.
What do you see in the future of femtech?
Meaningful, purposeful, and effective solutions. Holistic solutions that streamline and simplify tools/support/tech to the issues that matter most to women. These might include:
- Enablers to improve clinical research by gathering data and partnering with research centres. There is a need to accelerate understanding and research in women’s health whether it leads to better supporting female athletes or better understanding risk factors and treatment outcomes for women.
- Solutions that optimise pre-post natal and menopause (beyond education and community support) are key. Women have an important role to play in the global economy. At present, we aren’t achieving our full potential. Femtech is pivotal in this space to ensure that those who want, can fully participate and perform in the workforce, whatever stage of life they are at.
- Remote tech: Health systems are under pressure, solutions that empower women to engage with maintenance/ prevention of their health outside of hospitals (e.g. at home annual testing) are transformational.
- Innovations for earlier disease (eg cancer) detection: these can help to reduce the need for traumatic and expensive surgeries and treatments.
How can digital tools impact the femtech market?
FemTech by its very name is reliant heavily on tech innovation. Real impact will be:
- significant builds on current solutions that improve health outcomes and / or the female experience, OR
- carving out new solutions to unmet need spaces.
Leveraging nascent digital tools and optimising them for the female market (keeping this customer group at the heart of design, production and experience) will be critical to maximise impact.

Dr. Pamela Walker
News
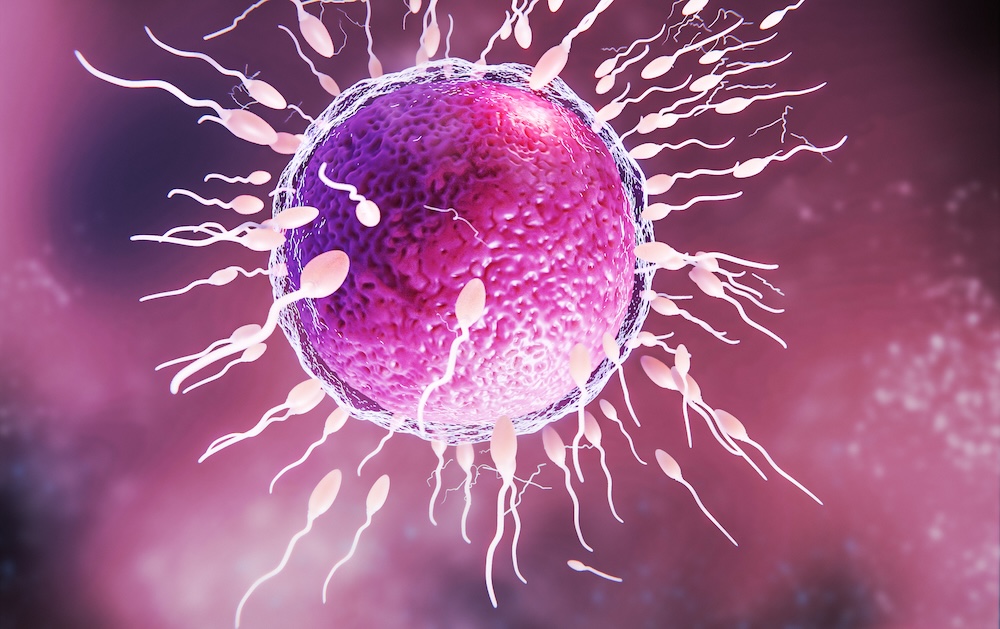
Can biotech help close the fertility gap? Inside the race to improve egg quality

With delayed parenthood now the norm, a new wave of biotech innovators is targeting the root cause of rising infertility rates. Oxford-based startup Uploid tells Femtech World how addressing egg ageing could reduce the “age penalty” that currently defines fertility outcomes.
Infertility now affects an estimated one in six people worldwide, with the World Health Organization determining it to be a “major public health issue.”
Across the OECD, the average age of first-time mothers has risen consistently over the past decades, driven by economic pressures, career progression, delayed partnership, and the availability of contraception. But human biology has not kept pace with this societal shift.
Egg quality declines sharply with age, beginning as early as the mid-thirties. It is this decline, not the body’s ability to carry a pregnancy, that remains the most significant factor behind falling conception rates.
IVF attempts to work around this challenge, yet even with technological advances, success rates remain modest. For women aged 18-34, birth rates per embryo transfer were around 35 per cent in 2022, dropping to five per cent by the age of 43-43.
“Fertility outcomes fall, not because the body is unable to sustain a pregnancy, but because egg quality declines with age,” Dr Alexandre Webster, co-founder and chief scientific officer at Oxford-based biotech firm, U-Ploid, tells Femtech World.
“Most existing fertility treatments are limited in how directly they can address this biological constraint. While IVF has advanced significantly in helping clinicians identify embryos with the best chance of success, there are currently very few options to intervene earlier and improve the quality of the eggs themselves.”
Current fertility treatments tend to focus on hormonal stimulation to produce more eggs, improving embryo selection, or improving implantation rates through uterine optimisation.
But none of these approaches address the root cause of age-related infertility, which is the egg’s declining ability to divide its chromosomes correctly.
This unmet need has set the stage for a new generation of reproductive biotech innovators, focusing on novel therapeutics, cellular engineering, AI-driven diagnostics, and biomarkers that could change how infertility is understood and treated.
A new frontier in fertility treatment
Among these innovators, U-Ploid is pioneering a new therapeutic category with Lyvanta™, a first-of-its-kind drug aimed at improving egg quality by addressing the biological mechanisms of maternal ageing.
Central to its approach is meiotic aneuploidy, which occurs when chromosomes fail to separate correctly as an egg matures. This increases dramatically with age, Webster explains, and is the leading cause of failed IVF cycles, miscarriage, and natural infertility. Studies have shown that over 50–80 per cent of embryos from women in their early 40s exhibit chromosomal abnormalities.
Lyvanta™ is designed to reduce the risk of these errors at the egg stage, before fertilisation occurs. It is injected into the egg before IVF, where it acts to stabilise chromosome segregation during meiosis.
“What makes this approach distinct is that, today, there are no approved or clinically available therapies that directly address meiotic aneuploidy or improve egg quality at its biological source,” Webster says.
“Lyvanta™ therefore represents a genuinely new therapeutic category. It does not act on embryos, does not alter DNA, and does not involve genetic modification. Instead, it supports a natural biological process that becomes increasingly error-prone with age.”
Evidence-gathering and regulatory engagement
The programme is grounded in over a decade of global academic research in chromosome biology and maternal ageing, and Uploid has carried out mechanistic studies, preclinical validation in aged animal models, and tightly regulated human egg studies in collaboration with IVF clinics.
However, the drug is still in the early stages of development, and the company is taking a cautious, evidence-driven approach.
Over the next one to two years, the research team will focus on building the scientific evidence needed to demonstrate clinical safety and efficacy. Meanwhile, regulatory engagement is ongoing, and timelines will depend on the outcomes of these studies.
“As with any new therapeutic, progress toward the clinic requires careful, stepwise evidence generation and regulatory review,” Webster says.
“Our focus at this stage is on ensuring that any future progress happens within established scientific, ethical, and regulatory frameworks. We engage with regulators, clinicians, and patient stakeholders to understand expectations around safety, evidence, transparency, and consent, and to ensure that the questions being asked of a new reproductive therapeutic are addressed rigorously and appropriately.”
He adds: “Lyvanta™ will only move forward if it meets the required standards set by regulators and ethics bodies, and only following thorough evaluation.”
If successful, the impact could be considerable. Improved egg quality may mean fewer IVF cycles, more viable embryos, and overall better outcomes for patients.
“If a therapy like Lyvanta™ can safely improve egg quality, it could lead to more viable embryos per IVF cycle, fewer cycles needed to achieve pregnancy, and better outcomes for people whose chances of success currently decline sharply with age,” Webster says.
“While much work remains, this is the long-term impact we are working toward.”
Global access and affordability
Globally, infertility affects people at similar rates regardless of income, but access to advanced treatments is often dependent on financial barriers.
IVF remains expensive worldwide. In the UK and US, a complete IVF cycle typically costs several thousand to tens of thousands of pounds, often requiring multiple attempts.
“One of the reasons fertility treatment is so costly and emotionally taxing is that patients often require multiple IVF cycles to achieve a successful outcome,” says Webster.
“Indeed, some 70 per cent of couples that start an IVF journey will end it with no baby, having run out of money and patience before a successful outcome.
By making each IVF cycle more efficient, it could reduce some of these costs and make treatment more accessible to more people.
“By improving egg quality upstream, Lyvanta™ has the potential to increase efficiency per cycle, which could reduce the overall burden, financial, physical, and emotional, on patients and healthcare systems,” Webster says.
The therapy is also being designed to integrate into existing IVF workflows, without requiring new infrastructure or highly specialised equipment.
He adds: “By focusing on improving biological efficiency rather than adding complexity, we believe this approach has the potential to support broader access over time, including in low- and middle-income countries where need is high but resources are limited.”
The new wave of fertility innovation
U-Ploid is part of a new wave of fertility biotech innovators. Companies such as Oxolife, developing a first-in-class oral drug to improve implantation; Gameto, engineering ovarian support cells to optimise IVF and egg freezing; and Genie Fertility, uncovering molecular biomarkers to personalise reproductive care, are all reshaping the field.
While progress in the fertility space has been incremental for decades, breakthroughs in chromosome biology, cell engineering, and molecular therapeutics are changing what might be possible.
This new generation of therapeutic innovation could improve outcomes and expand options for millions navigating delayed parenthood, and allow fertility science to catch up with the realities of modern life.
“Our aim is to reduce the biological ‘age penalty’ that currently defines fertility outcomes, so that success is less tightly coupled to chronological age,” Webster adds.
“If successful, this could allow more people to build families on timelines that reflect modern social and economic realities.”
Insight
Women face worse stroke recovery than men in first year, study finds
Insight
Caesarean births overtake natural vaginal deliveries in England for first time

Caesarean births (surgical births) have overtaken vaginal deliveries in England for the first time, with 45 per cent of births now by caesarean, NHS data show.
Last year, 44 per cent of births were through natural vaginal deliveries and 11 per cent were assisted with instruments such as forceps or ventouse, according to data published on Tuesday covering April 2024 to March 2025. Assisted deliveries use instruments to help the baby out during birth.
More than four in ten caesareans carried out by NHS England were elective, planned operations. For women under 30, natural vaginal birth remained the most common method, while for women aged 30 and over, caesareans were most common. For women aged 40 and over, 59 per cent of births were by caesarean.
In total, 20 per cent of births in 2024-25 were planned caesareans and 25.1 per cent were emergency, with both figures at record highs.
There were 542,235 deliveries in NHS England hospitals during this period, down from 636,643 in 2014-15. One in four births were to mothers aged over 35.
In 2014-15, caesarean deliveries made up 26.5 per cent of births. The increase over the past decade has been attributed to growing numbers of complex pregnancies, linked to factors including rising obesity rates and women waiting until they are older to have children.
Donna Ockenden, one of the UK’s most senior midwives who is leading the inquiry into maternity failures in Nottingham, told BBC Radio 4’s Today programme that the rise was a “complex” and “evolving picture over time”.
She said: “The thousands of women I’ve spoken to want a safe birth above everything else, so we should not vilify or criticise women who make those decisions.”
“In the reality of today’s maternity services – where women are living in poverty, deprivation, they’ve got pre-existing illnesses – obstetricians, midwives, nurses can only do so much, and we don’t always do enough in all cases to optimise women’s health prior to pregnancy.”
Soo Downe, a professor of midwifery at the University of Lancashire, added: “In some cases women are going for caesarean sections as a kind of least-worst option because they don’t really believe they’re going to have the kind of support they need to have a safe, straightforward, positive labour and birth in hospital.
“Or because their birth centres are being closed … or because they go into labour wanting a home birth and the midwife isn’t able to come to them because the midwife’s called somewhere else.
“But for some of them, it becomes the only choice on the table … and for other women, they choose a caesarean because they really want one, and that’s absolutely fine.”
-

 Features1 week ago
Features1 week agoCannabis compounds kill ovarian cancer without harming healthy cells, research finds
-

 Insight3 weeks ago
Insight3 weeks agoFemtech in 2025: A year of acceleration, and what data signals for 2026
-

 News4 weeks ago
News4 weeks agoInnovate UK relaunches £4.5m women founders programme
-

 Insight2 weeks ago
Insight2 weeks agoMeta removes dozens of abortion advice and queer advocacy accounts
-

 News3 weeks ago
News3 weeks agoRound up: First wearable detects symptoms of perimenopause, and more
-

 Insight2 weeks ago
Insight2 weeks agoSperm donor with cancer-causing gene fathered nearly 200 children across Europe
-

 Mental health3 weeks ago
Mental health3 weeks agoInsomnia combined with sleep apnea associated with worse memory in older women
-

 Insight4 weeks ago
Insight4 weeks agoCanada targets US$37bn femtech opportunity




























3 Comments