Fertility
Clinical trial of device aims to induce ovulation in women with polycystic ovary syndrome

Physicians are leading a national clinical trial to help women with polycystic ovary syndrome (PCOS)-related infertility who want to become pregnant.
The trial, called REBALANCE, studies the safety and effectiveness of an investigational device developed by May Health that is designed to restore ovulation disrupted by PCOS.
OU Health reproductive endocrinologist Karl Hansen, M.D., Ph.D., chair of the Department of Obstetrics and Gynecology at the OU College of Medicine, is leading the trial for OU and was the first physician in the United States to use the device.
“Polycystic ovary syndrome is a common endocrine disorder that affects about 10% of all women of reproductive age,” said reproductive endocrinologist Karl Hansen at the University of Oklahoma Health Sciences in Oklahoma City .
“And it is the most common cause of infertility related to the absence of ovulation. It is exciting to be studying a new potential treatment option for women with PCOS-related infertility.
“It also highlights the importance of academic medicine. We’re not here to only provide the care that we already know; we’re here to push the envelope and develop new understandings and treatments.”
PCOS is a hormonal imbalance that occurs when the ovaries release an excess of androgens, a sex hormone that plays a central role in reproductive health. The overproduction of androgens sparks a series of events that result in irregular ovulation or the absence of it.
Hansen said about 80 per cent of women with PCOS respond to oral medications designed to stimulate ovulation, and up to 50 per cent of those women will achieve a pregnancy. However, approximately 20 per cent of women do not begin ovulating with the medications.
An alternative treatment involves gonadotropin injections, which require frequent monitoring and precise dosage adjustments. Another option, laparoscopic ovarian drilling, uses a needle-like device inserted through small abdominal incisions to deliver laser or radiofrequency energy to an ovary, aiming to restore ovulation.
However, this procedure has become less common, Hansen said.
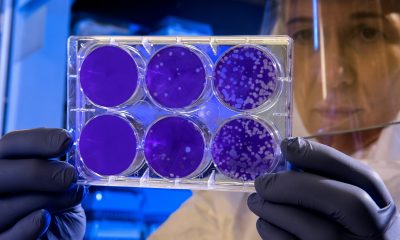
The investigational device from May Health aims to prompt ovulation in women with PCOS-related infertility through a minimally invasive outpatient procedure. The device is connected to a probe commonly used in transvaginal ultrasounds, which assesses the ovary before delivering electrothermal energy to perform the appropriate number of ablations on an ovary.
The REBALANCE trial will enrol approximately 195 patients with PCOS-related infertility at multiple sites across the United States.
Researchers will assess how often women ovulate after the procedure. Secondary outcomes that will be measured include the pregnancy rate achieved after the procedure, other symptoms of PCOS, and how long the effects of the procedure endure.
OU Health Sciences is co-leading the trial in conjunction with the University of Pennsylvania.
“We are glad to be partnering with May Health to offer this trial to patients with PCOS-related infertility,” Hansen said.
“Most women with PCOS come to us because they are trying to get pregnant. For the subset of women who do not respond to oral medications, this is an exciting development to evaluate this investigational device.”
News
Woman files lawsuit claiming fertility clinic ‘bootcamp’ caused her stroke

A London executive is suing a fertility clinic, alleging its IVF treatment led to her suffering a stroke.
Navkiran Dhillon-Byrne, 51, began private IVF treatment at the Assisted Reproduction and Gynaecology Centre (ARGC) in Wimpole Street, London, in April 2018.
Ten days after her treatment ended, on 28 April 2018, she suffered a stroke, which her lawyers say has left her with ongoing vision problems.
Ms Dhillon-Byrne is now suing the clinic and its head, Mohamed Taranissi, for negligence and breach of duty, saying medics failed to give her sufficient warnings about stroke risks linked to IVIg immunotherapy (intravenous immunoglobulin) – a one-off add-on treatment designed to moderate the body’s immune responses during pregnancy.
The clinic and Dr Taranissi deny liability, saying Ms Dhillon-Byrne was fully informed of the risks.
They also dispute that IVIg caused her stroke.
Central London County Court heard that Ms Dhillon-Byrne, chief marketing officer at the City of London base of an international software company, turned to private treatment after the NHS was unable to fund her IVF in 2014.
She had an unsuccessful attempt at another London clinic before choosing ARGC. She told the court she had been trying to have a child since 2014.
She said she selected ARGC after a friend recommended it, praising what they described as high success rates.
The clinic’s website describes its approach as “IVF boot camp” and promotes “in-depth investigations, daily monitoring and real-time treatment adjustments.”
Ms Dhillon-Byrne says she was not warned of the “specific” risks of thrombosis – blood clotting that can lead to stroke – in relation to the IVIg therapy.
She also says the clinic overstated her chances of success and failed to secure her “informed consent” before treatment began.
She argues that, had she been given a clear picture of her chance of a successful pregnancy, she would not have consented to IVF and the supplemental IVIg therapy.
Denying Ms Dhillon-Byrne’s claims, the clinic’s KC, Clodagh Bradley, told the court that the success rate advice given was “accurate and in accordance with the ARGC data.”
She added that Ms Dhillon-Byrne had been informed that the immune treatment was new and “still controversial.”
Lawyers said outside court that, if successful, Ms Dhillon-Byrne’s claim is likely to be worth “millions” due to the impact of the stroke on her high-flying career.
The trial continues.
Fertility
YON E Health raises €250k for its vaginal health device

Dutch femtech startup Yon E Health has raised €250k in pre-seed funding to develop a smart vaginal health sensor that measures pH and temperature.
The device will monitor key indicators linked to fertility, infection risk and reproductive wellbeing, tackling what the company says are long-standing gaps in women’s healthcare.
Founded by Roswitha Verwer in 2022, the Amsterdam-based startup is creating an at-home medical device for continuous pH and basal body temperature tracking.
pH levels show the acidity of the vaginal environment, with changes often signalling infections or fertility shifts.
Basal body temperature monitoring helps to identify ovulation patterns.
Roswitha Verwer, founder and CEO, said: “When I started Yon E, I was told vaginal health was too taboo, too complex, and too ‘niche’ for innovation and investment.
“That’s what motivated and pushed me even more.
“For too long, women have had to guess, self-diagnose, or wait until they show symptoms and something goes wrong with their health.
“We’re changing that, turning silence into data women can actually use.”
The raise follows a surge in investor interest in European femtech this year.
UK-based Hormona secured €7.8m for its hormone-tracking platform, while France’s Solence raised €1.6m for AI-based PCOS digital therapeutics. S
SheMed closed a €43m round for its personalised health platform, and Unfabled has reached around €3m in total funding for its women’s health platform.
Currently, vaginal pH testing relies on single-use paper strips, usually used after symptoms appear.
Yon E Health’s sensor aims to allow at-home monitoring of both pH and basal body temperature at once, helping spot early warning signs of imbalance and improve timing for conception.
The round was led by PMK-Group, with support from UniPrisma Venture Studio partners Károly Szántó and Thijmen Meijer, who guided term sheet development.
Matias Toye, founder of Oyster Shield and Dilicheck, provided M&A and fundraising support.
“Vaginal health isn’t a luxury; it’s a foundation of overall wellbeing,” said Dr Muskaan Bhan, chief clinical officer at Yon E Health.
“Our technology bridges the gap between research and reality, empowering women globally with real-time, clinical-grade insights that can prevent complications before they start.”
The company says less than 1 per cent of global medical research funding is directed at conditions specific to women, and only 2.3 per cent of venture capital went to female-founded startups in 2024.
Vaginal pH imbalance can indicate conditions such as bacterial vaginosis (an overgrowth of bacteria), yeast infections, fertility issues and hormonal changes.
Yon E Health’s technology is designed to give women and clinicians better visibility into menstrual cycles, microbiome health and fertility windows.
Yon E Health has a multidisciplinary team across Amsterdam, Budapest, London, Texas, Boston and Madrid.
The pre-seed funding will support preparations for medical trials – a step towards clinical and consumer launch.
News
Researchers achieve first pregnancy using AI to recover sperm in infertile men
Researchers have reported the first successful pregnancy using an AI-guided sperm recovery method in infertile men with azoospermia, a condition where ejaculate contains little or no sperm.
The case involved a man who had spent nearly 20 years trying to start a family, undergoing multiple IVF cycles, manual sperm searches and two surgical procedures.
Male factors account for around 40 per cent of infertility in couples, and 10–15 per cent of infertile men have azoospermia.
Researchers at Columbia University Fertility Center developed the technique, detailed in a research letter published online on 31 October 2025.
Zev Williams is senior author and director of the Columbia University Fertility Center.
Williams said: “A semen sample can appear totally normal, but when you look under the microscope you discover just a sea of cellular debris, with no sperm visible.”
Many couples with male-factor infertility are told they have little chance of having a biological child.
Men with azoospermia may undergo a procedure to have sperm surgically extracted from the testes, but the procedure is often unsuccessful and can cause vascular problems, inflammation or a temporary drop in testosterone.
Currently, a few specialist labs manually inspect semen samples — a slow and expensive process — often after centrifugation or other treatments that can damage sperm.
“The field has really been challenged to find a better way to identify and retrieve viable sperm cells in men with exceedingly low sperm counts,” Williams said.
The new approach, called STAR (Sperm Tracking and Recovery), combines imaging, microfluidics and AI to identify and recover rare sperm cells from men with azoospermia.
The method uses high-powered imaging to scan semen samples, taking more than eight million images in under an hour.
AI then pinpoints sperm cells, and a microfluidic chip – a device with tiny, hair-like channels – isolates the portion containing sperm.
Within milliseconds, a robot gently removes the sperm so it can be used to create an embryo or frozen for later use.
Hemant Suryawanshi is assistant professor of reproductive sciences at Columbia University Vagelos College of Physicians and Surgeons and project leader.
Suryawanshi said: “Our team included experts in advanced imaging techniques, microfluidics, and reproductive endocrinology to tackle each step required to find and isolate rare sperm.”
STAR was tested in a patient who provided a 3.5 mL semen sample.
Within about two hours, it scanned 2.5 million images and identified two viable sperm cells, which were used to create two embryos and start a pregnancy.
“You only need one healthy sperm to create an embryo,” Williams said.
Although based on a single case, the findings demonstrate the feasibility of using this technology to help men with azoospermia overcome long-standing barriers to biological parenthood.
Larger clinical studies are now under way to assess STAR’s efficacy in broader patient populations.
The research team first unveiled the STAR method earlier this year, combining advanced imaging and microfluidic technologies to detect and extract rare sperm cells.
Once identified, the system can remove sperm within milliseconds for immediate use or freezing.
-

 News3 weeks ago
News3 weeks agoDozens of women report suffering painful burns after using Always sanitary towels
-

 Entrepreneur4 weeks ago
Entrepreneur4 weeks agoWomen’s health innovations recognised in TIME’s Best Inventions 2025
-

 Entrepreneur3 weeks ago
Entrepreneur3 weeks agoCutting through the noise in femtech – key takeaways from Women’s Health Week 2025
-

 News4 weeks ago
News4 weeks agoMenstrual cycle affects women’s reaction time, study finds
-

 News2 weeks ago
News2 weeks agoAI embryo selection tool wins European approval
-

 News3 weeks ago
News3 weeks agoScientists develop breakthrough approach to detecting endometriosis in menstrual blood
-

 Menopause2 weeks ago
Menopause2 weeks agoTestosterone patch shows promise for menopausal women
-

 Entrepreneur2 weeks ago
Entrepreneur2 weeks agoFrom SEO to GEO: How women’s health brands can get found in the age of AI